Development of the respiratory system
Lung development involves 5 stages:
- Embryonic
- Pseudoglandular
- Canalicular
- Saccular
- Alveolar
Tip: Remember those stages with “Every Pulmonologist Can See Alveoli!”
Embryonic stage (weeks 4–7)
In the embryonic stage, the trachea and the primary bronchial buds develop.
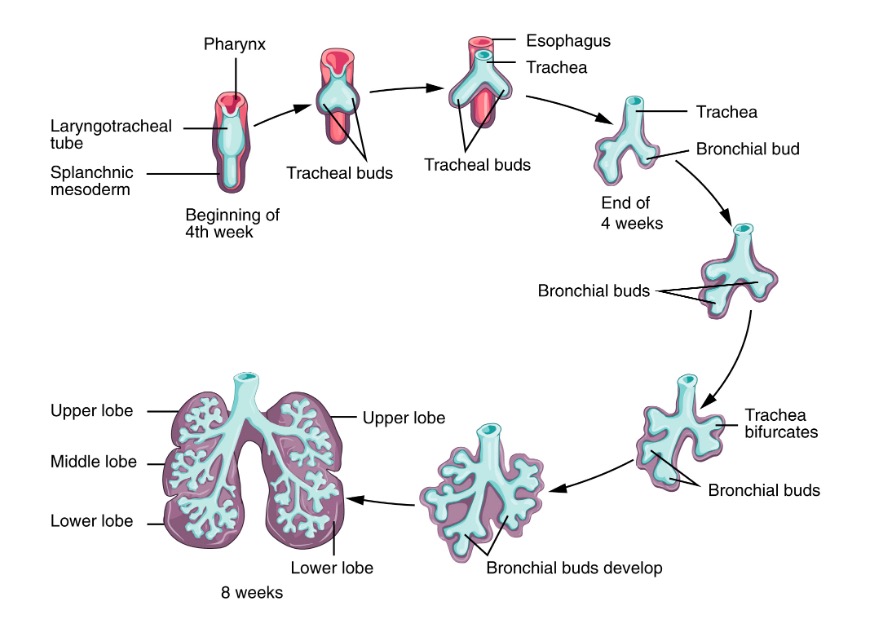
Early stage of lung development:
During the early stages of lung development (embryonic and pseudoglandular), the lung bud gradually transforms into the trachea and then bifurcates, forming the two mainstem bronchi. These bronchi will further divide, giving rise to lobar and segmental bronchi.
Pseudoglandular stage (weeks 5–16)
Main steps of the pseudoglandular stage involve the development of the bronchial tree.
Note: The first breathing movement can be detected around 10 weeks of gestation, however, since the respiratory bronchioles don’t develop until the next stage, the fetus cannot survive at this point yet.
Canalicular stage (weeks 16–26)
In this stage, the respiratory units (canaliculi) develop. By the end of the canalicular stage, the fetus is capable of enough respiration to survive with intensive care.
Saccular stage (week 26 until birth)
In the saccular stage, the alveoli begin to mature, capillary networks grow, and surfactant production increases significantly.
Alveolar stage (32 weeks until 8 years of age)
The respiratory units grow and mature further throughout this time: goes from 50 million alveoli at birth to 300 million by age 8 (with rapid increase in the first 6 months).
Differences between children’s and adult’s respiratory system
Tip: As we know, children are not just “small adults.” Their physiology and anatomy varies in significant ways that require specialized treatment and open up the possibility for different conditions than adults are affected by.
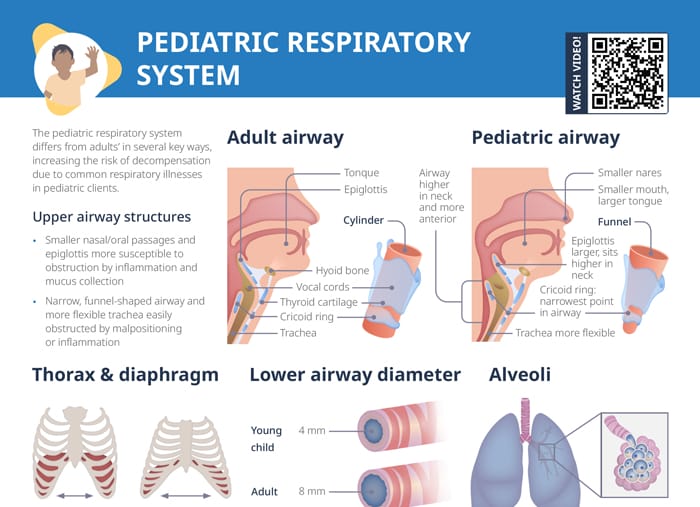
Pediatric vs adult upper airway
- Children have smaller nasal/oral passages
- Children’s epiglottis is larger and sits higher in the neck → more susceptible to obstruction by inflammation and mucus collection
- Children’s airway is narrow, funnel-shaped; trachea is more flexible → easily obstructed by malpositioning or inflammation
Pediatric vs adult lower airway
- Children’s airway diameter is smaller (4 mm vs adult’s 8 mm).
- Patency easily compromised by bronchoconstriction and mucus collection
- Immature beta-adrenergic receptors less responsive to bronchodilator medications
Pediatric vs adult thorax and diaphragm
In children, the diaphragm fatigues more easily. The accessory muscles are immature and weaker, and the increased rib cage angle and relatively large organ size limit chest expansion. Increasing the respiratory rate is the only mechanism to increase lung function in children.
Pediatric vs adult alveoli
At birth, children have a much smaller number of functioning alveoli, so the area for gas exchange is much smaller. The small, immature alveoli are more susceptible to collapse and atelectasis.
Pediatric vs adult surfactant
Lung surfactant is a phospholipid produced within the alveoli that reduces surface tension and keeps the alveoli open. It is produced at 30–34 weeks gestation and will be insufficient in premature infants.
Insufficient surfactant may cause:
- Increased surface tension
- Difficulty expanding alveoli
- Increased work of breathing
- Atelectasis
- Lung collapse
Pediatric respiratory assessment
History
- Present illness (symptoms, progression, etc)
- Past medical history (asthma, pneumonia, allergies, etc)
- Family/social history (passive smoke exposure, asthma in the family)
Inspection
- General inspection (alertness, irritability)
- Respiratory rate, rhythm, depth, quality, work of breathing
- Symmetry of breathing
Palpation
- Skin temperature/integrity
- Lymph nodes
- Abnormal movements, bulges
- Tenderness
- Symmetric chest expansion
- Tactile fremitus
Percussion
Tone should be flat over bony structures, organs, and muscles, resonant over lung tissue.
Auscultation
- Equality of lung sounds bilaterally
- Air exchange
Related videos
Abnormal findings in a pediatric respiratory assessment
Inspection:
- Irritability (unconsolable)
- Blueness to lips or mucus membranes
- Retractions
- Nasal flaring
- Grunting
- High-pitched sounds on expiration
- Increased respiratory rate
Palpation:
- Enlarged lymph nodes
- Localized tenderness
- Asymmetric chest expansion (pneumothorax or pneumonia)
- Increased tactile fremitus (pneumonia)
- Decreased tactile fremitus (asthma)
Percussion:
Dull sound over lung fields can indicate pneumonia or other lung infiltrations.
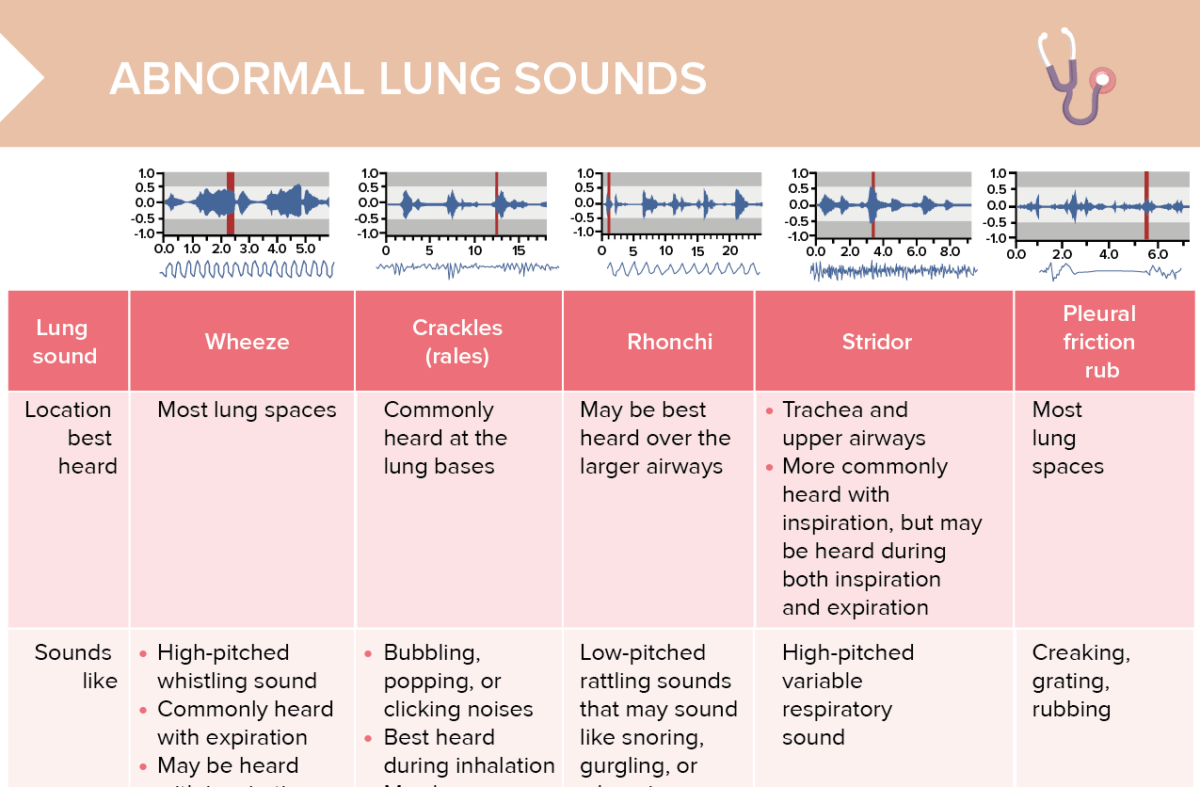
Auscultation:
- Wheezing
- Crackles
- Rhonchi
- Stridor
- Cough