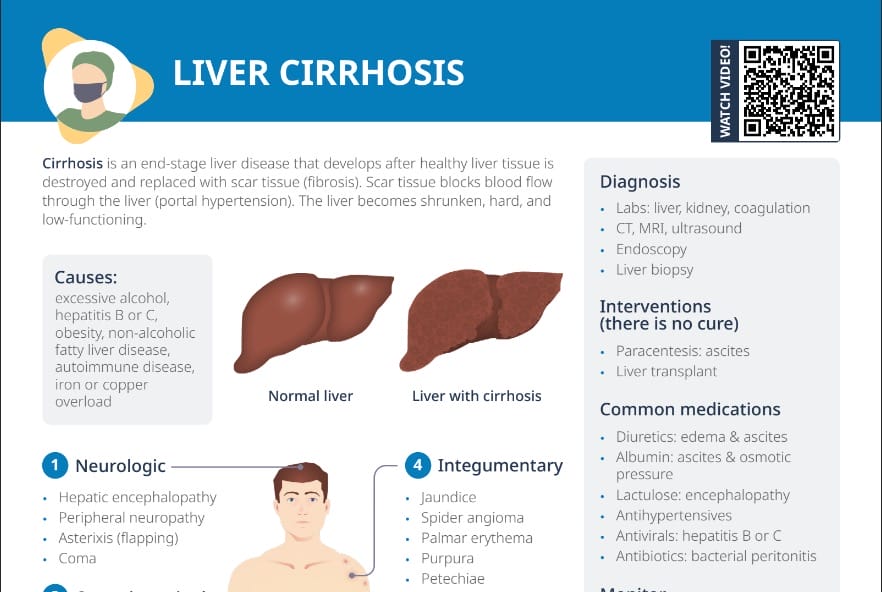
What is liver cirrhosis?
Liver cirrhosis is an end-stage liver disease that develops after healthy liver tissue is destroyed and replaced with scar tissue (fibrosis).
Common causes of liver cirrhosis
The common causes of liver cirrhosis include:
- Excessive alcohol consumption
- Hepatitis B or C
- Obesity
- Non-alcoholic fatty liver disease
- Autoimmune disease
- Iron or copper overload
Symptoms of liver cirrhosis
The symptoms of liver cirrhosis include:
- Neurologic:
- Hepatic encephalopathy
- Peripheral neuropathy
- Asterixis
- Coma
- Gastrointestinal:
- Anorexia
- Dyspepsia
- Nausea, vomiting
- Change in bowel habits
- Dull abdominal pain
- Fetor hepaticus
- Esophageal and gastric varices
- Melena
- Gastritis
- Hematemesis
- Rectal varices
- Reproductive:
- Gynecomastia
- Testicular atrophy
- Impotence
- Amenorrhea
- Integumentary:
- Jaundice
- Spider angioma
- Palmar erythema
- Purpura
- Petechiae
- Caput medusae
- Hematologic:
- Anemia
- Thrombocytopenia
- Leukopenia
- Coagulation disorders
- Splenomegaly
- Metabolic:
- Hypokalemia
- Hyponatremia
- Hypoalbuminemia
- Cardiovascular:
- Fluid retention
- Peripheral edema
- Ascites
Click here for a step-by-step walkthrough of an NCLEX practice question about liver cirrhosis ➜
Related videos
Potential complications
Potential complications of liver cirrhosis include hepatic encephalopathy, peripheral neuropathy, asterixis (flapping), coma, bacterial peritonitis, and variceal bleeding.
What is variceal bleeding?
Variceal bleeding occurs when blood vessels in the esophagus or stomach, dilated due to portal hypertension, rupture and bleed. When blood is blocked to the liver by clots or scar tissue, the esophageal varices (veins in the lining of the esophagus) cannot accommodate the normal blood volume and will burst, resulting in a life-threatening bleeding episode. Management includes urgent endoscopy, administration of vasoactive drugs, antibiotics to prevent infection, and in some cases, placement of a TIPS (transjugular intrahepatic portosystemic shunt).
How is liver cirrhosis diagnosed?
Liver cirrhosis is diagnosed through a combination of physical examination, laboratory tests (including liver, kidney, and coagulation tests), imaging tests (such as CT, MRI, and ultrasound), endoscopy, and liver biopsy.
What are interventions for liver cirrhosis?
There is no cure for liver cirrhosis. Management focuses on treating the underlying cause, preventing further liver damage, managing complications, and maintaining quality of life. Nurses play a pivotal role in client education (including dietary guidance), medication administration, symptom monitoring, and emotional support.
Potential interventions are:
- Diuretics, albumin, lactulose, antihypertensives, antivirals, and antibiotics to help manage symptoms and prevent complications
- Paracentesis for ascites
- In severe cases, a liver transplant may be necessary.
Note: Diuretics such as spironolactone or furosemide are commonly used to manage ascites by reducing fluid accumulation. Nurses should monitor for side effects like electrolyte imbalances (particularly low potassium levels), dehydration, and renal function impairment.
Client education: How can people with liver cirrhosis manage their symptoms and prevent complications?
Clients can manage their symptoms and maintain a healthy lifestyle by avoiding hepatotoxic medications, consuming a well-balanced, sodium-restricted diet, scheduling periods of rest, maintaining a healthy weight, and engaging in mild exercise. Alcohol and smoking should be avoided.
Clients should be advised to monitor their stools and emesis for blood, elevate their legs to mobilize edema/ascites, and seek medical attention if they experience any changes in their mental status, bleeding, or edema/abdominal girth.
What is the MELD score?
The MELD (Model for End-Stage Liver Disease) score is a reliable measure of mortality risk in clients with end-stage liver disease and is used to prioritize persons with liver disease for receiving a liver transplant. It takes into account bilirubin, creatinine, and the INR for prothrombin time.
Liver cirrhosis nursing diagnoses
For liver cirrhosis, potential nursing diagnoses include:
- Chronic confusion: monitor for signs of encephalopathy, provide safe environment
- Defensive coping: regarding stopping substance abuse
- Fatigue
- Imbalanced nutrition: less than body requirements (anorexia and malabsorption; encourage small, frequent meals)
- Nausea: due to gastric irritation
- Chronic pain: liver enlargement
- Risk for bleeding: decreased synthesis of clotting factors by the liver and esophageal varices; monitor for signs for bleeding
- Risk for injury: with intoxication and delirium tremens