What is incentive spirometry?
Incentive spirometry is a breathing therapy technique aiming to improve lung function and prevent respiratory complications. It involves having the patient inhale deeply through a spirometer (a handheld device with a series of chambers and a visual indicator) while holding it at a predetermined level, encouraging them to take slow and deep breaths.
Incentive spirometer purpose
The goals of incentive spirometry include expanding lung capacity, improving oxygen exchange, and maintaining healthy lung function.
Incentive spirometry indications
Incentive spirometry is often applied in postoperative care, especially after surgeries involving the chest or abdomen, as well as in managing various respiratory conditions.
Incentive spirometer instructions
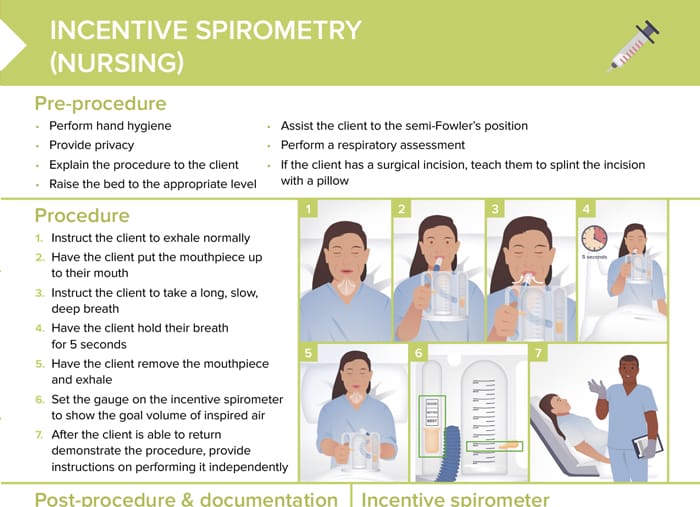
Pre-procedure: preparing incentive spirometry
- Perform hand hygiene
- Provide privacy
- Explain procedure
- Raise bed to appropriate level
- Assist client to semi-Fowler’s position
- Perform respiratory assessment
- If client has a surgical incision, teach them to splint incision with a pillow
Procedure: how to instruct a client to use a spirometer
- Instruct the client to exhale normally
- Have the client put the mouthpiece up to their mouth
- Instruct the client to take a long, slow, deep breath while watching the piston go up
- Have the client hold their breath for 5 seconds
- Have the client remove the mouthpiece and exhale
- Set the gauge on the incentive spirometer to show the goal volume of inspired air
- After the client is able to return demonstrate the procedure, provide instructions on performing it independently
Post-procedure and how to document a spirometry
- Reassess client’s respiratory status
- Return the bed to the lowest position
- Perform hand hygiene
- Document the procedure
Be sure to document:
- Maximum inspiration volume
- Number of times it was used
Notify the healthcare provider if:
- Client experiences any signs of respiratory distress
- Volume obtained differs significantly from previous measurements
- If the client is unable to achieve the inspiratory goal
Peak flow meter vs incentive spirometer
A peak flow meter measures how fast a patient can blow air out of their lungs, helping in monitoring conditions, such as asthma.
An incentive spirometer does not measure exhalation, but helps the patient to take slow, deep breaths with the aim of improving lung function.
How often to use incentive spirometer
Clients should follow providers’ instructions on frequency of spirometer use. For example, a client may be instructed to take several breaths with the spirometer every hour.
How long to use incentive spirometer after surgery
The duration of incentive spirometer use after surgery varies depending on the patient’s condition and healthcare provider’s instructions. Often, it is used in the immediate postoperative period for a few days to a week.