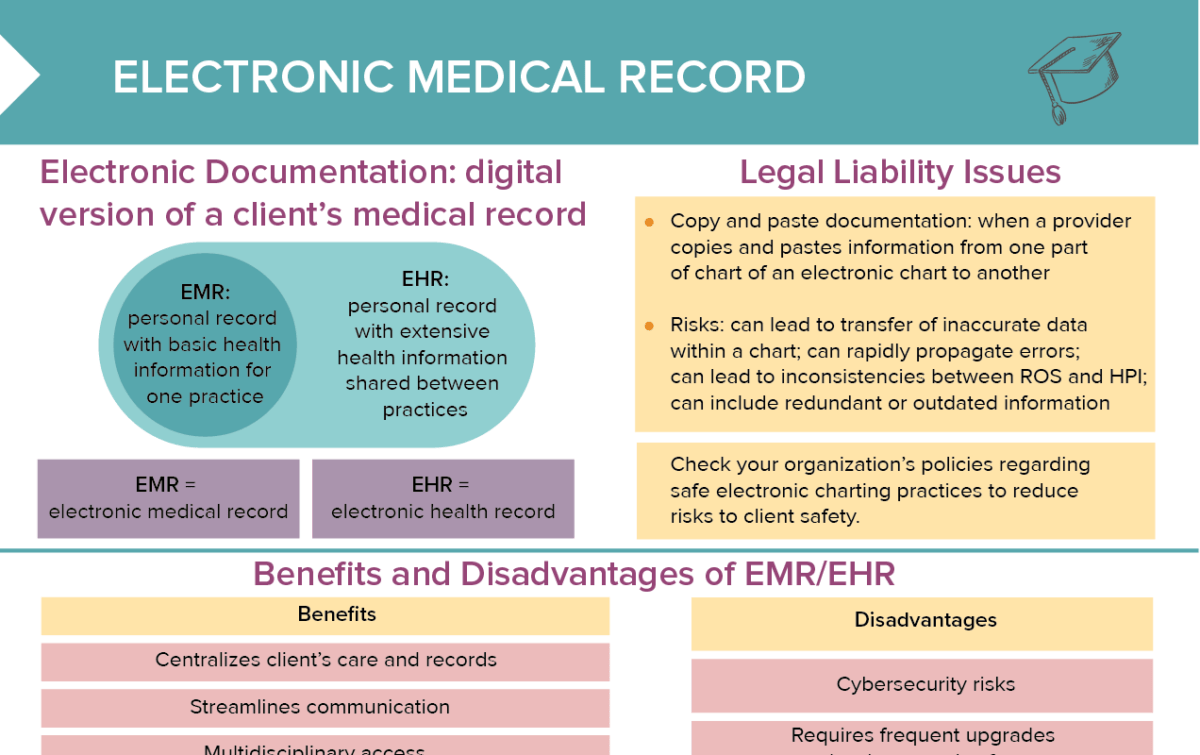
What is an electronic medical record (EMR)?
An electronic medical record is a personal record for a client with basic health information, created by one practice.
What is an electronic health record (EHR)?
An electronic health record is a personal record for a client with extensive health information which is shared between different practices treating a client.
EMR vs EHR: What is the difference?
The terms EMR and EHR are used interchangeably by some, but they are different things.
An EMR is created by one medical practice about a client that is treated there and kept as a record for this client.
EHRs are more in-depth and are not only used in one practice, but shared with other healthcare providers treating the client.
Which legal issues do nurses need to pay attention to?
Check your organization’s policies regarding safe electronic charting practices to reduce risks to client safety.
Copy-pasting in EMRs/EHRs
When a provider copies and pastes information from one part of a chart of an electronic chart to another, this can lead to the transfer of inaccurate data within a chart, rapidly propagating errors. Copy-pasting can also lead to inconsistencies between ROS and HPI, and lead to documentation including redundant or outdated information.
Electronic signatures and data integrity
Make sure to use your own unique login credentials and never share them with anyone else. Never alter or delete another person’s entries; and correct your own errors transparently.
How are corrections made to the electronic medical record?
Correction procedures vary by system and facility, but there are some general rules:
- The original entry is never deleted, but kept for documentation.
- A new note is made indicating the error and the correct information.
- Date and time of the correction and context must be provided.
HIPAA compliance rules for EMR/EHR
Authorization
Employees only have access to minimum necessary information.
Authentication
Each user must log in individually and only have access to appropriate records.
Automatic logoff
Sessions need to be terminated after a period of inactivity.
Audits and alerts
Each user’s activity needs to be automatically logged at all times.
Encryption
All data must be encrypted.
Hosting and infrastructure
HIPAA-compliant hosting platforms must be used.
Business associate addendum
Any 3rd party providers with access to client information must sign a BAA contract.
Advantages and disadvantages of EHR/EMR
Advantages of using EHR/EMR
- Centralizes client’s care and records
- Streamlines communication
- Multidisciplinary access
- Allows flagging, trending and screening of client status
- Facilitates direct client care (MAR, allergy checks, etc.)
- Reduces medical errors
- Increases availability of data for research
Disadvantages of using EHR/EMR
- Cybersecurity risks
- Requires frequent upgrades to hardware and software
- Technology failures can lead to inability to access records.
- Technical support required
- Privacy concerns, increased access from staff