Definition: What is angina pectoris?
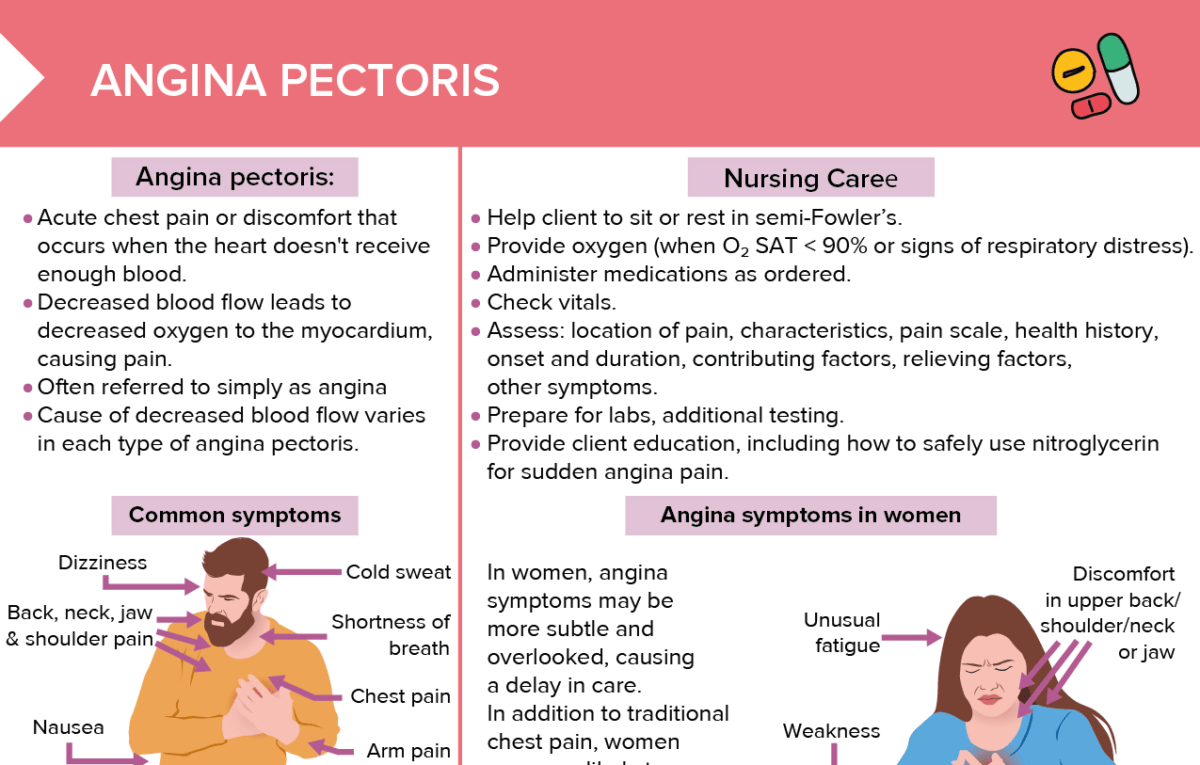
Angina pectoris ( “angina”, acute chest pain or discomfort) occurs when the heart doesn’t receive enough blood.
ICD-10 code for angina pectoris
The ICD-10 code for angina pectoris is I20.
- I20.0: Unstable angina
- I20.1: Angina pectoris with documented spasm
- I20.8: Other forms of angina pectoris
- I20.9: Angina pectoris, unspecified
What causes chest pain?
Decreased blood flow leads to decreased oxygen to the myocardium, causing pain. The cause of decreased blood flow varies in each type of angina pectoris.
Types of angina pectoris and their causes
| Type | Cause | Characteristics |
| Stable | Fixed stenosis (demand ischemia) | Triggered by exertion, stress, cold exposure, coronary artery disease Relieved by rest or medication Predictable and consistent |
| Unstable | Thrombus (supply ischemia) | May occur at rest or with exertion Worsens over time May not be relieved by rest or medication Lasts longer than 20 minutes, may go away and come back |
| Variant Prinzmetal | Vasospasm (supply ischemia) | Occurs most commonly at night, during rest/sleep Relieved by medication |
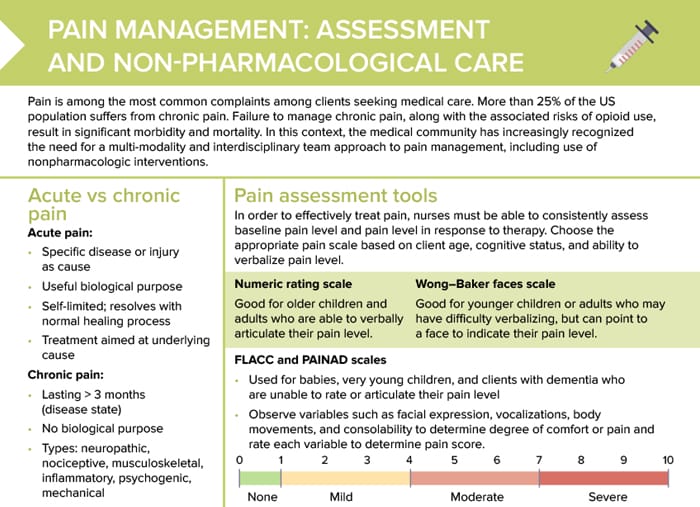
Angina pectoris symptoms
- Chest pain
- Arm pain
- Dizziness
- Back. neck, jaw and shoulder pain
- Cold sweat
- Shortness of breath
- Nausea
Angina symptoms in women
In women, angina symptoms may be more subtle and overlooked, causing a delay in care. In addition to traditional chest pain, women are more likely to experience these symptoms:
- Unusual fatigue
- Discomfort in upper back/shoulder/neck or jaw
- Abdominal pain and nausea
- Weakness
What are the ECG changes associated with angina pectoris?
Understanding ECG changes associated with angina pectoris is essential for nurses to recognize, such as:
- Detect heart-related conditions early on
- Effectively monitor clients to be able to act quickly
- Communicate effectively with clients and health care team about significance of ECG changes
- Assess response to treatment
Possible ECG changes due to angina pectoris:
- ST segment depression (indicating ischemia)
- T wave inversion (suggesting ischemia)
- Pathological Q waves (previous myocardial infarction, associated with coronary heart disease)
Note: EKG may be normal in clients with angina pectoris, especially when currently no symptoms are experienced.
Nursing diagnoses for chest pain
- Acute pain: assess pain, administer prescribed pain medication, teach client about importance of rest
- Ineffective tissue perfusion: related to compromised coronary blood flow; monitor and provide medications (nitrates or beta blockers may be prescribed)
- Anxiety or death anxiety: provide reassurance
- Activity intolerance: assess, encourage gradual increase in activity, teach energy conservation techniques
- Knowledge deficit: client education about disease, medications, lifestyle modifications
Angina pectoris nursing interventions
- Help client to sit or rest in semi-Fowler’s
- Provide oxygen (when O₂ SAT < 90% or signs of respiratory distress)
- Administer medications as ordered
- Check vitals
- Assess: location of pain, characteristics, pain scale, health history, onset and duration, contributing factors, relieving factors, other symptoms
- Prepare for labs, additional testing
- Provide client education, including how to safely use nitroglycerin for sudden angina pain
Emergency management steps for chest pain
If O2 SAT < 90% or in respiratory distress:
- M: Morphine
- O: Oxygen
- N: Nitrates
- A: Aspirin
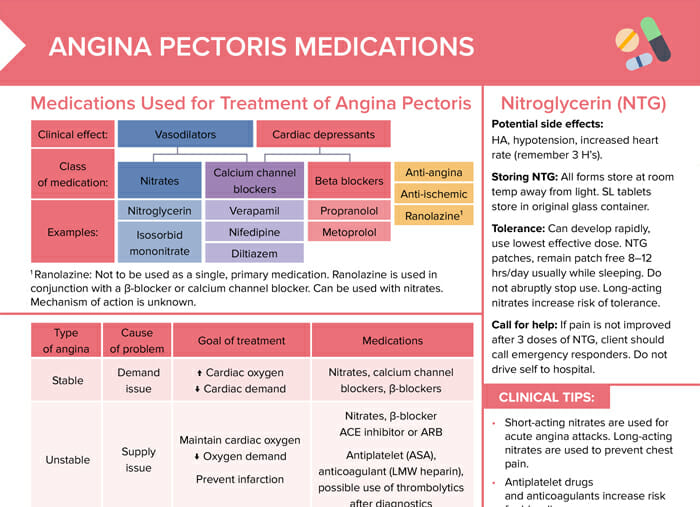
Angina pectoris medications
Clinical tips
- Short-acting nitrates are used for acute angina attacks. Long-acting nitrates are used to prevent chest pain.
- Antiplatelet drugs and anticoagulants increase risk for bleeding.
- β-blockers are not used in variant angina. They can increase risk of coronary artery spasm.
Medications used for treatment of chest pain
- Nitrates (nitroglycerin, isosorbid mononitrate): vasodilation
- Calcium channel blockers (verapamil, nifedipine, diltiazem): vasodilation, cardiac depressants
- Beta blockers (propranolol, metoprolol): cardiac depressants
Bonus download:
Medications for angina pectoris
Review of medications used for acute and stable angina
Types of angina pectoris and their management
| Type | Goal of treatment | Medications |
| Stable | Increase cardiac oxygen, decrease cardiac demand | Nitrates, calcium channel blockers, β-blockers |
| Unstable | Maintain cardiac oxygen, decrease oxygen demand, prevent infarction | Nitrates, β-blocker, CE inhibitor or ARB, antiplatelet (ASA), anticoagulant (LMW heparin), possible use of thrombolytics after diagnostics |
| Variant Prinzmetal | Increase cardiac oxygen | Nitrates, calcium channel blockers |