What is a blood transfusion?
A blood transfusion is a medical procedure where a client receives donated blood or blood products into their bloodstream. It’s typically used to replace blood lost due to surgery or injury, or when the body cannot produce blood properly because of an illness. A health care provider orders the transfusion and a consent is signed by the client.
How do blood transfusions work?
Blood transfusions involve introducing donated blood or blood components (like red blood cells, plasma, or platelets) into a patient’s bloodstream through an intravenous (IV) line. The body uses the donated blood as if it was its own, using the red cells for oxygen transport, platelets to aid clotting, and plasma for various functions including clotting and immunity.
Why would someone need a blood transfusion?
Indications for blood transfusions include:
- Severe blood loss (e.g., from major injury, surgery)
- Anemia (e.g., due to kidney disease, cancer)
- Hematologic conditions (e.g., sickle cell disease)
- Planned transfusions during certain treatments (e.g., bone marrow transplant)
- Disease or chemotherapy agent causing a lack of certain blood components (e.g., platelets)
What RBC level requires a blood transfusion?
There’s no set hemoglobin level/RBC count that universally requires a blood transfusion. However, according to guidelines from the American Association of Blood Banks (AABB), a transfusion is often considered when the hemoglobin level is less than 7 to 8 grams per deciliter in stable, non-bleeding patients.
How many blood transfusions can a cancer patient have?
The number of blood transfusions a patient diagnosed with cancer can have depends on their individual condition, the type and stage of cancer, and the treatment they’re undergoing. Some patients may require multiple transfusions over a period of time due to anemia caused by chemotherapy or the cancer itself. Each transfusion must be considered individually to balance its potential benefit against its risks.
How long does a blood transfusion take?
A blood transfusion typically takes 1–4 hours for one unit of blood, but this can vary depending on the specific situation.
Why do Jehovah’s witnesses refuse blood transfusions?
Jehovah’s witnesses refuse blood transfusions based on religious beliefs that another’s blood is not used to sustain life. It’s important for healthcare providers to respect these beliefs and explore alternative treatment options, whenever possible.
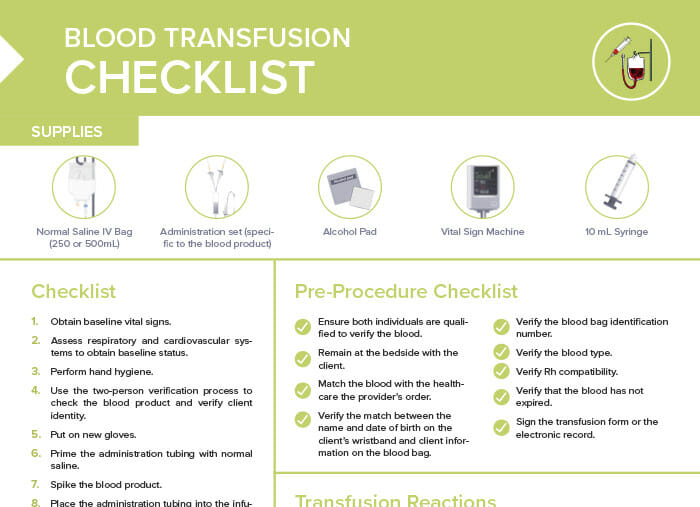
What supplies are needed for blood transfusions?
- Normal saline IV bag
- Administration set (specific to the blood product)
- Alcohol pad
- Vital sign machine
- 10-mL syringe
Nursing tips for blood transfusions: important considerations
Pre-procedure considerations
- Some individuals have religious preferences that do not allow them to receive blood products.
- Typically, blood samples drawn for compatibility (type and screen) are good for 72 hours only.
- A physician or licensed independent practitioner (LIP) should obtain consent from the client (not a nurse).
- Don’t let the blood product sit for > 30 minutes before beginning administration.
- Blood must be completely infused within 4 hours.
- If there is an order to give medications with the transfusion…
- … administer oral medications (e.g., Benadryl) 30 minutes before starting transfusion.
- … administer intravenous (IV) medications immediately before starting transfusion.
- IV catheters should be patent and of the correct size.
- Never infuse any other medications in the same tubing as that of the blood.
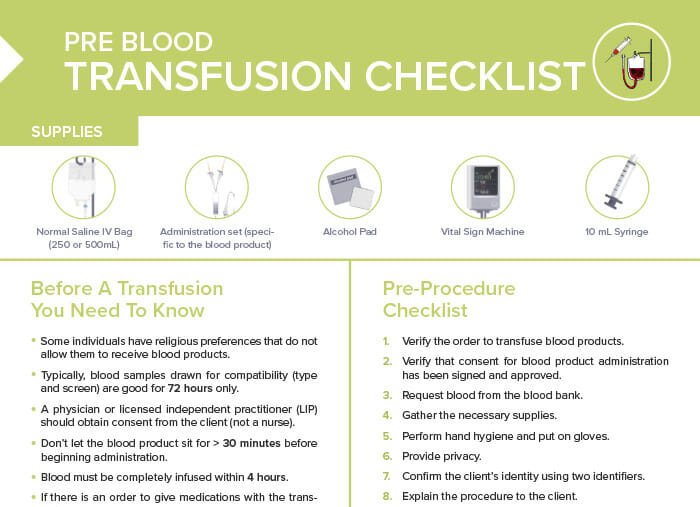
Bonus download: pre-blood transfusion checklist
Bring this with you when getting ready to administer a blood transfusion and never forget one of the prep steps again!
Blood transfusion checklist: procedure
- Obtain baseline vital signs.
- Assess respiratory and cardiovascular systems to obtain baseline status.
- Use the two-person verification process to check the blood product and verify client identity.
- Perform hand hygiene.
- Put on non-sterile gloves.
- Prime the administration tubing with normal saline.
- Spike the blood product.
- Place the administration tubing into the infusion pump.
- Use an alcohol pad to scrub the hub of the peripheral IV tubing.
- Flush the peripheral IV with normal saline using a 10 mL syringe.
- Attach the administration set to the peripheral IV tubing.
- Label the tubing near the client for quick identification.
- Begin infusion at a low rate (30-50mL/hr) and remain at bedside for 15 minute monitoring period.
- Stay with the client during the first 15 minutes of infusion to monitor for transfusion reactions.
- After 15 minutes, perform respiratory and cardiovascular assessments and recheck the vital signs of the client. After the first 15 minutes, monitor the client per agency protocols.
- Increase the infusion rate as prescribed.
- If a transfusion reaction or infiltration is observed, stop the infusion and notify the provider.
What are transfusion reactions?
Transfusion reactions are adverse events that occur during or after a blood transfusion. They can include:
- Respiratory:
- Dyspnea
- Rales (lung sounds)
- Pulmonary edema
- Cardiovascular:
- Tachycardia
- Hypotension
- Jugular vein distention
- Other:
- Fever
- Flank pain
- Pruritus
- Dermatitis
Note: DO NOT flush the line if a patient transfusion reaction is suspected to avoid any further blood product administration.
Why is it important to know a person’s Rhesus factor before a blood transfusion?
The Rhesus (Rh) factor is a specific protein found on the surface of red blood cells. People are either Rh positive (have the protein) or Rh negative (don’t have the protein). Before a blood transfusion, it’s vital to know a person’s Rh factor to prevent a possible immune response.