What are anticholinergics?
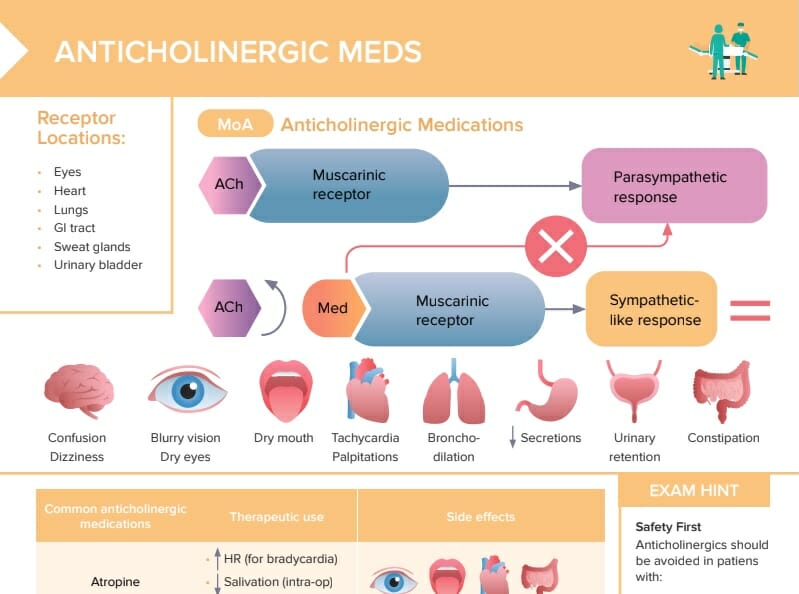
Anticholinergic medications are a group of drugs that block the action of acetylcholine, a neurotransmitter that transmits signals in the nervous system.
These medications target the cholinergic system, which is involved in a wide range of functions including muscle movement, heart rate, digestion, salivation, and other processes. Anticholinergics work by blocking the muscarinic acetylcholine receptors, thereby inhibiting parasympathetic nerve impulses. This can have a variety of effects on the body, depending on the specific drug and dosage.
How do anticholinergics work?
When acetylcholine binds to muscarinic receptors, it leads to various physiological responses such as muscle contraction, heart rate reduction, increased secretions, etc. By blocking these receptors, anticholinergic medications inhibit these actions. This results in various therapeutic effects, depending on where the receptors are located.
- In the lungs: bronchodilation
- In the gastrointestinal tract: reduce motility and secretions
- In the urinary tract: decrease bladder muscle contractions
- In the eyes: pupil dilation
- In the heart: increase heart rate
What are the receptor locations of anticholinergic medications?
Anticholinergic medications primarily target muscarinic acetylcholine receptors. Receptor locations:
- Eyes
- Heart
- Lungs
- GI tract
- Sweat glands
- Urinary bladder
List of common anticholinergic drugs and their therapeutic uses
Anticholinergic medications are a diverse group, used to treat a variety of conditions. Here are some common examples:
- Atropine: for bradycardia, reduce salivation and bronchial secretions during surgery, and as an antidote for organophosphate poisoning
- Oxybutynin: bladder relaxant (for overactive bladder)
- Ipratropium (inhaled anticholinergics): used in inhaler form for bronchodilation (COPD, asthma)
- Scopolamine: for motion sickness and postoperative nausea and vomiting
- Solifenacin: bladder relaxant (for overactive bladder)
What are the potential side effects of anticholinergic medications?
Table: Anticholinergics side effects
| Medication | Side effects |
| Atropine | Blurry vision/dry eyes, dry mouth, tachycardia/palpitations, constipation |
| Oxybutynin | Blurry vision/dry eyes, urinary retention, constipation, H/A |
| Ipratropium | Confusion/dizziness, dry mouth, urinary retention, constipation, N/V |
| Scopolamine | Confusion/dizziness, dry mouth, sweating, sore throat |
| Solifenacin | Dry mouth, urinary retention, N/V, bladder pain, cloudy urine |
Which clients should not be given anticholinergic medications?
Anticholinergics should be avoided in clients with:
- Myasthenia gravis
- Glaucoma
- Tachycardia, HTN
- Increased age
- Hyperthyroidism
- Heart failure
- Severe dry mouth/constipation
- Liver disease
- Enlarged prostate
- Hiatal hernia