Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Diagnosis of meningitis is made on clinical grounds with a thorough neurologic examination. CSF analysis is an important diagnostic tool, as it is difficult to identify the exact cause clinically. Management of meningitis includes immediate broad-spectrum antibiotics and supportive therapy to prevent complications. Specific treatment depends on the etiology of meningitis. Delay in treatment can lead to permanent neurologic defects and death.
Last updated: Mar 4, 2024
Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis is inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body’s defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation of the protective membranes of the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification and the spinal cord Spinal cord The spinal cord is the major conduction pathway connecting the brain to the body; it is part of the CNS. In cross section, the spinal cord is divided into an H-shaped area of gray matter (consisting of synapsing neuronal cell bodies) and a surrounding area of white matter (consisting of ascending and descending tracts of myelinated axons). Spinal Cord: Anatomy, collectively called the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy, that is commonly caused by an acute infection.
Meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis can be of infectious (most common) or noninfectious origin. Infectious meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis can be community- or hospital-acquired.
Bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis:
Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis:
Fungal meningitis Fungal meningitis Meningitis caused by fungal agents which may occur as opportunistic infections or arise in immunocompetent hosts. Meningitis:
Parasitic meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis:

3-dimensional (3D) image of a group of diplococcal gram-negative Neisseria meningitidis
Image: “A 3D image of a group of diplococcal, Gram-negative, Neisseria meningitidis, bacteria” by Centers for Disease Control and Prevention. License: Public DomainDirect inoculation of the infectious agent into the meninges Meninges The brain and the spinal cord are enveloped by 3 overlapping layers of connective tissue called the meninges. The layers are, from the most external layer to the most internal layer, the dura mater, arachnoid mater, and pia mater. Between these layers are 3 potential spaces called the epidural, subdural, and subarachnoid spaces. Meninges: Anatomy is rare in meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis. Usually, infection at an adjacent or remote site spreads to the brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification.
Acute meningitis Acute Meningitis Meningitis:
Chronic meningitis Chronic Meningitis Meningitis:
The clinical features of bacterial and viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis are similar. Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis tends to be less acute and usually self-limits within 7–10 days.
The classic triad presenting in ~50% of bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis cases is:[2–8]
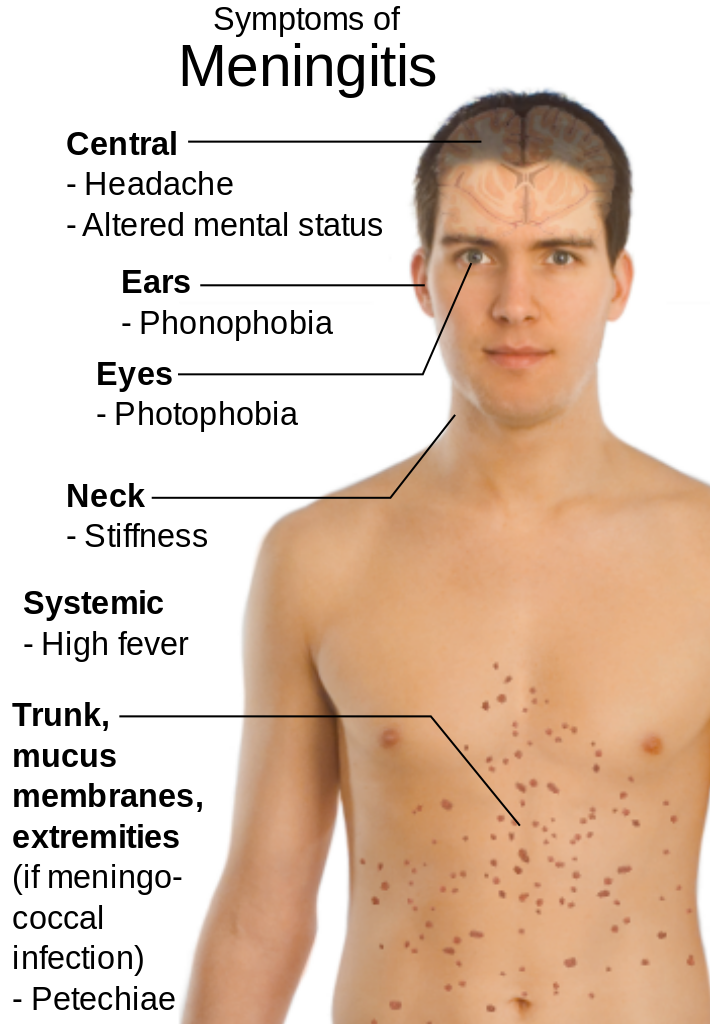
Clinical presentation of meningitis
Image: “Main symptoms of Meningitis” by Mikael Häggström. License: Public DomainCommence empiric antibiotics immediately after obtaining blood cultures and CSF samples. If lumbar puncture Lumbar Puncture Febrile Infant is delayed, obtain blood cultures and administer antibiotics until it can safely be performed.
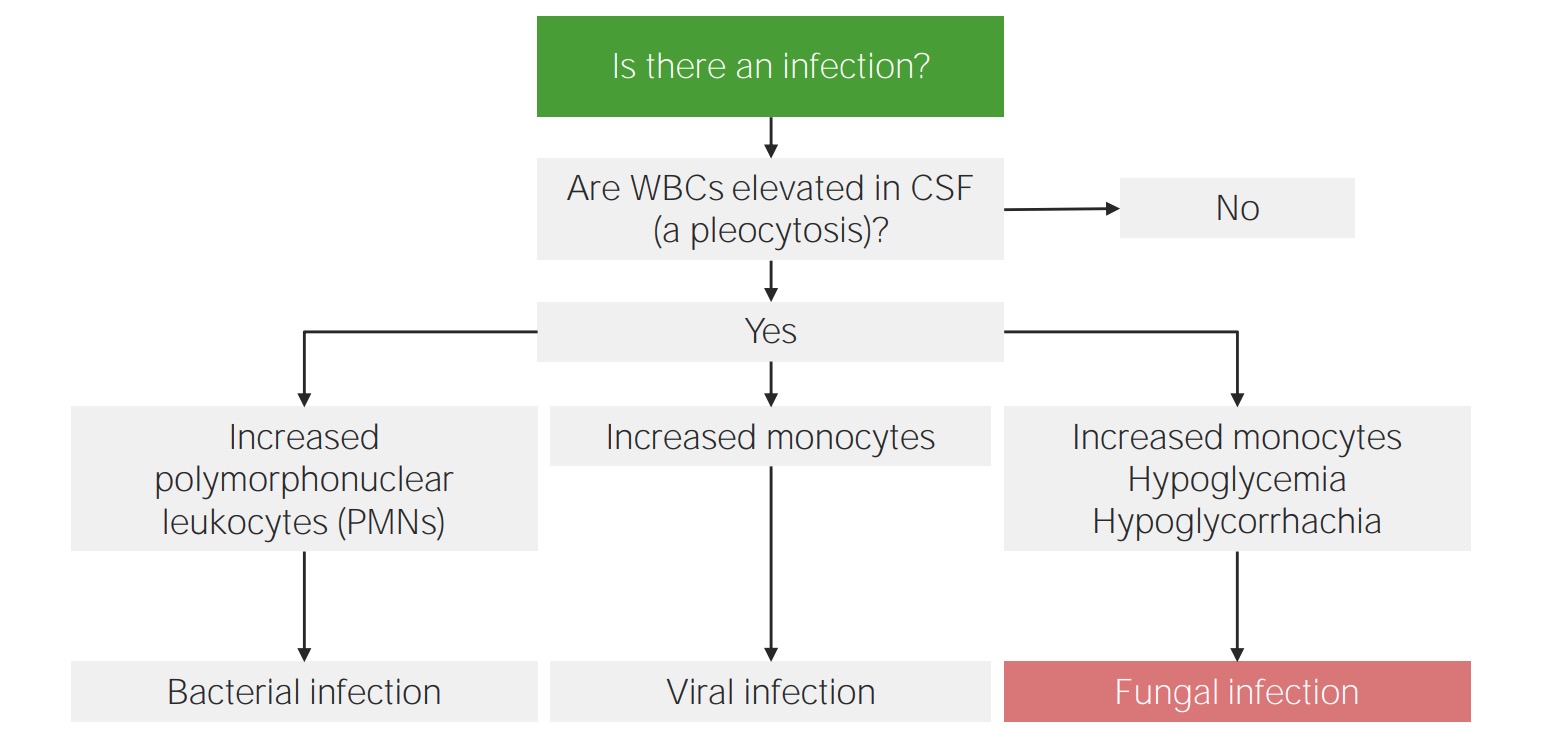
Approach to CSF analysis in meningitis:
Differential count is the key to identifying the etiology of meningitis.
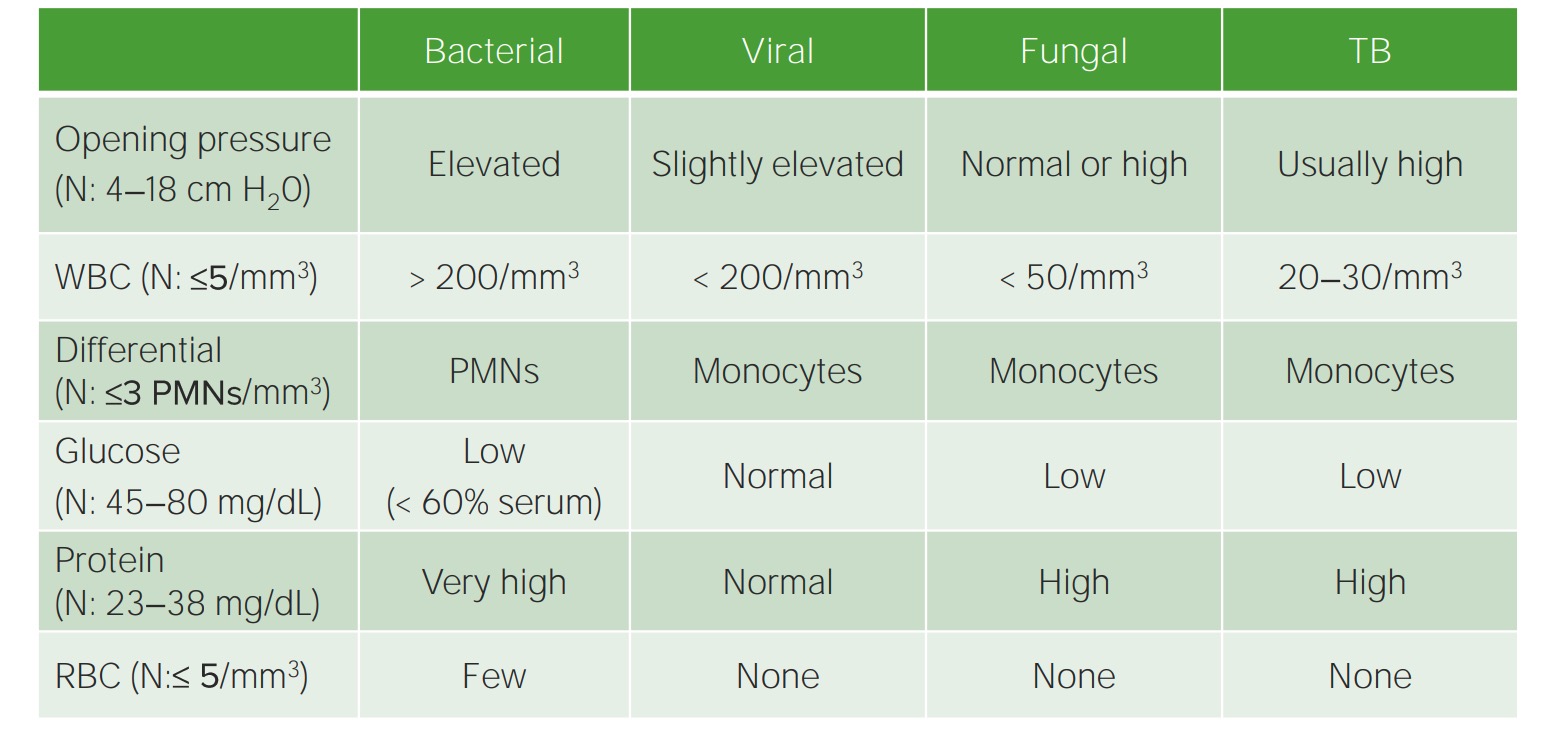
Parameters of CSF analysis in meningitis
N: NormalImaging is not required for diagnosis but is usually indicated before performing a lumbar puncture Lumbar Puncture Febrile Infant if there is a concern about high intracranial pressure Intracranial Pressure Idiopathic Intracranial Hypertension and to detect complications.
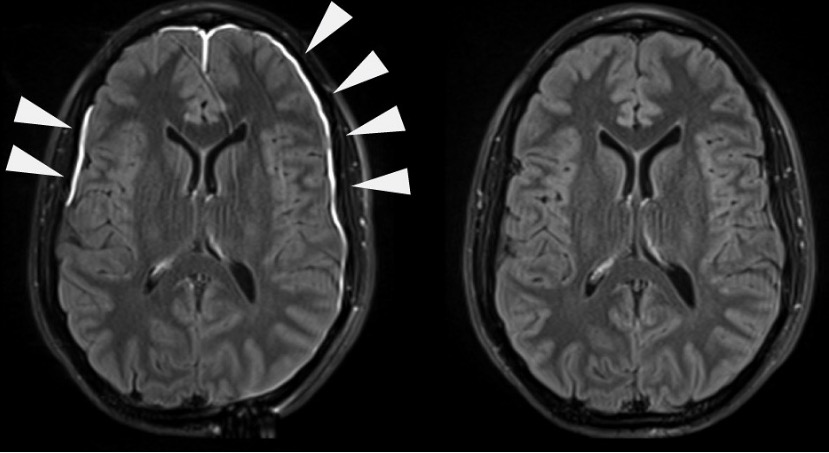
Meningeal irritation evident on contrast-enhanced MRI
Image: “Damaged Meninges” by National Institutes of Health (NIH). License: Public DomainTreatment is based on the type of meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis. The patient should always be stabilized first using the A-E approach. Supportive care is common for most patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship. Broad-spectrum Broad-Spectrum Fluoroquinolones antibiotics are usually administered as an immediate measure while the cause is being determined.
US guidelines:
UK guidelines:
Initial supportive measures:
Bacterial meningitis Bacterial meningitis Bacterial infections of the leptomeninges and subarachnoid space, frequently involving the cerebral cortex, cranial nerves, cerebral blood vessels, spinal cord, and nerve roots. Meningitis:
| Factors | Bacteria Bacteria Bacteria are prokaryotic single-celled microorganisms that are metabolically active and divide by binary fission. Some of these organisms play a significant role in the pathogenesis of diseases. Bacteriology | Antibiotics |
|---|---|---|
| Age < 1 month | S. pneumoniae, N. meningitidis N. meningitidis A species of gram-negative, aerobic bacteria. It is a commensal and pathogen only of humans, and can be carried asymptomatically in the nasopharynx. When found in cerebrospinal fluid it is the causative agent of cerebrospinal meningitis. It is also found in venereal discharges and blood. There are at least 13 serogroups based on antigenic differences in the capsular polysaccharides; the ones causing most meningitis infections being a, b, c, y, and w-135. Each serogroup can be further classified by serotype, serosubtype, and immunotype. Neisseria, S. agalactiae, E. coli, H. influenzae H. influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through VIII. Haemophilus | Ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins + cefotaxime Cefotaxime Semisynthetic broad-spectrum cephalosporin. Cephalosporins OR ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins + aminoglycoside ( gentamicin Gentamicin Aminoglycosides) |
| Age 1–23 months | S. agalactiae, E. coli, L. monocytogenes L. monocytogenes A species of gram-positive, rod-shaped bacteria widely distributed in nature. It has been isolated from sewage, soil, silage, and from feces of healthy animals and man. Infection with this bacterium leads to encephalitis, meningitis, endocarditis, and abortion. Listeria Monocytogenes/Listeriosis, Klebsiella Klebsiella Klebsiella are encapsulated gram-negative, lactose-fermenting bacilli. They form pink colonies on MacConkey agar due to lactose fermentation. The main virulence factor is a polysaccharide capsule. Klebsiella pneumoniae is the most important pathogenic species. Klebsiella spp. | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + 3rd-generation cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections |
| Age 2–50 years | S. pneumoniae, N. meningitidis N. meningitidis A species of gram-negative, aerobic bacteria. It is a commensal and pathogen only of humans, and can be carried asymptomatically in the nasopharynx. When found in cerebrospinal fluid it is the causative agent of cerebrospinal meningitis. It is also found in venereal discharges and blood. There are at least 13 serogroups based on antigenic differences in the capsular polysaccharides; the ones causing most meningitis infections being a, b, c, y, and w-135. Each serogroup can be further classified by serotype, serosubtype, and immunotype. Neisseria | |
| Age > 50 years | S. pneumoniae, N. meningitidis N. meningitidis A species of gram-negative, aerobic bacteria. It is a commensal and pathogen only of humans, and can be carried asymptomatically in the nasopharynx. When found in cerebrospinal fluid it is the causative agent of cerebrospinal meningitis. It is also found in venereal discharges and blood. There are at least 13 serogroups based on antigenic differences in the capsular polysaccharides; the ones causing most meningitis infections being a, b, c, y, and w-135. Each serogroup can be further classified by serotype, serosubtype, and immunotype. Neisseria, L. monocytogenes L. monocytogenes A species of gram-positive, rod-shaped bacteria widely distributed in nature. It has been isolated from sewage, soil, silage, and from feces of healthy animals and man. Infection with this bacterium leads to encephalitis, meningitis, endocarditis, and abortion. Listeria Monocytogenes/Listeriosis, aerobic gram-negative bacilli Bacilli Shigella | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins + 3rd-generation cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections |
| Basilar skull Skull The skull (cranium) is the skeletal structure of the head supporting the face and forming a protective cavity for the brain. The skull consists of 22 bones divided into the viscerocranium (facial skeleton) and the neurocranium. Skull: Anatomy fracture Fracture A fracture is a disruption of the cortex of any bone and periosteum and is commonly due to mechanical stress after an injury or accident. Open fractures due to trauma can be a medical emergency. Fractures are frequently associated with automobile accidents, workplace injuries, and trauma. Overview of Bone Fractures | S. pneumoniae, H. influenzae H. influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through VIII. Haemophilus, group A β-hemolytic streptococci | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + 3rd-generation cephalosporin Cephalosporin Multidrug-resistant Organisms and Nosocomial Infections |
| Penetrating trauma | S. aureus S. aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Staphylococcus, coagulase-negative staphylococci Coagulase-negative staphylococci Staphylococcus, aerobic gram-negative bacilli Bacilli Shigella (including Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas) |
Vancomycin
Vancomycin
Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear.
Glycopeptides +
ceftazidime
Ceftazidime
Semisynthetic, broad-spectrum antibacterial derived from cephaloridine and used especially for pseudomonas and other gram-negative infections in debilitated patients.
Cephalosporins OR Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + cefepime Cefepime A fourth-generation cephalosporin antibacterial agent that is used in the treatment of infections, including those of the abdomen, urinary tract, respiratory tract, and skin. It is effective against pseudomonas aeruginosa and may also be used in the empiric treatment of febrile neutropenia. Cephalosporins OR Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Postneurosurgery | Aerobic gram-negative bacilli Bacilli Shigella (including P. aeruginosa P. aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas), S. aureus S. aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Staphylococcus, coagulase-negative staphylococci Coagulase-negative staphylococci Staphylococcus | |
| CSF shunt | S. aureus S. aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Staphylococcus, coagulase-negative staphylococci Coagulase-negative staphylococci Staphylococcus, aerobic gram-negative bacilli Bacilli Shigella (including P. aeruginosa P. aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas), Propionibacterium acnes Propionibacterium acnes A bacteria isolated from normal skin, intestinal contents, wounds, blood, pus, and soft tissue abscesses. It is a common contaminant of clinical specimens, presumably from the skin of patients or attendants. Acne Vulgaris | |
| Immunocompromised immunocompromised A human or animal whose immunologic mechanism is deficient because of an immunodeficiency disorder or other disease or as the result of the administration of immunosuppressive drugs or radiation. Gastroenteritis state (e.g., AIDS AIDS Chronic HIV infection and depletion of CD4 cells eventually results in acquired immunodeficiency syndrome (AIDS), which can be diagnosed by the presence of certain opportunistic diseases called AIDS-defining conditions. These conditions include a wide spectrum of bacterial, viral, fungal, and parasitic infections as well as several malignancies and generalized conditions. HIV Infection and AIDS, on immunosuppressive agents) | S. pneumoniae, L. monocytogenes L. monocytogenes A species of gram-positive, rod-shaped bacteria widely distributed in nature. It has been isolated from sewage, soil, silage, and from feces of healthy animals and man. Infection with this bacterium leads to encephalitis, meningitis, endocarditis, and abortion. Listeria Monocytogenes/Listeriosis, N. meningitidis N. meningitidis A species of gram-negative, aerobic bacteria. It is a commensal and pathogen only of humans, and can be carried asymptomatically in the nasopharynx. When found in cerebrospinal fluid it is the causative agent of cerebrospinal meningitis. It is also found in venereal discharges and blood. There are at least 13 serogroups based on antigenic differences in the capsular polysaccharides; the ones causing most meningitis infections being a, b, c, y, and w-135. Each serogroup can be further classified by serotype, serosubtype, and immunotype. Neisseria, aerobic gram-negative bacilli Bacilli Shigella (including P. aeruginosa P. aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas) | Vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins + cefepime Cefepime A fourth-generation cephalosporin antibacterial agent that is used in the treatment of infections, including those of the abdomen, urinary tract, respiratory tract, and skin. It is effective against pseudomonas aeruginosa and may also be used in the empiric treatment of febrile neutropenia. Cephalosporins OR vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides + meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam |
| Microorganism | IV antibiotics (adult dose) | Durationa |
|---|---|---|
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus pneumoniae |
Vancomycin
Vancomycin
Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear.
Glycopeptidesb 15–20 mg/kg every 8–12 hours + Ceftriaxone Ceftriaxone A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears. Cephalosporins 2 g every 12 hours Discontinue vancomycin Vancomycin Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear. Glycopeptides if ceftriaxone-susceptible. |
10–14 days |
| Neisseria meningitidis Neisseria meningitidis A species of gram-negative, aerobic bacteria. It is a commensal and pathogen only of humans, and can be carried asymptomatically in the nasopharynx. When found in cerebrospinal fluid it is the causative agent of cerebrospinal meningitis. It is also found in venereal discharges and blood. There are at least 13 serogroups based on antigenic differences in the capsular polysaccharides; the ones causing most meningitis infections being a, b, c, y, and w-135. Each serogroup can be further classified by serotype, serosubtype, and immunotype. Neisseria |
Ceftriaxone
Ceftriaxone
A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears.
Cephalosporins 2 g every 12 hours Other options (if susceptible): Penicillin Penicillin Rheumatic Fever G 4 mU every 4 hours OR Ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins 2 g every 4 hours |
7 days |
| Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus agalactiae (group B Streptococcus Streptococcus Streptococcus is one of the two medically important genera of gram-positive cocci, the other being Staphylococcus. Streptococci are identified as different species on blood agar on the basis of their hemolytic pattern and sensitivity to optochin and bacitracin. There are many pathogenic species of streptococci, including S. pyogenes, S. agalactiae, S. pneumoniae, and the viridans streptococci. Streptococcus) |
Ampicillin
Ampicillin
Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic.
Penicillins 2 g every 4 hours OR Penicillin Penicillin Rheumatic Fever G 4 mU every 4 hours |
14–21 days |
| Haemophilus influenzae Haemophilus Influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through viii. Haemophilus(β-lactamase–negative) | Ampicillin Ampicillin Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic. Penicillins 2 g every 4 hours | 7 days |
| Haemophilus influenzae Haemophilus Influenzae A species of Haemophilus found on the mucous membranes of humans and a variety of animals. The species is further divided into biotypes I through viii. Haemophilus(β-lactamase–positive) |
Ceftriaxone
Ceftriaxone
A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears.
Cephalosporins 2 g every 12 hours OR Cefotaxime Cefotaxime Semisynthetic broad-spectrum cephalosporin. Cephalosporins 2 g every 4–6 hours |
|
| Listeria Listeria Listeria spp. are motile, flagellated, gram-positive, facultative intracellular bacilli. The major pathogenic species is Listeria monocytogenes. Listeria are part of the normal gastrointestinal flora of domestic mammals and poultry and are transmitted to humans through the ingestion of contaminated food, especially unpasteurized dairy products. Listeria Monocytogenes/Listeriosis monocytogenes> |
Ampicillin
Ampicillin
Semi-synthetic derivative of penicillin that functions as an orally active broad-spectrum antibiotic.
Penicillins 2 g every 4 hours OR Penicillin Penicillin Rheumatic Fever G 4 mU every 4 hours Consider adding gentamicin Gentamicin Aminoglycosides 1.7 mg/kg every 8 hours for synergy.c |
≥ 21 days |
| E. coli(and other Enterobacteriaceae Enterobacteriaceae A family of gram-negative, facultatively anaerobic, rod-shaped bacteria that do not form endospores. Its organisms are distributed worldwide with some being saprophytes and others being plant and animal parasites. Many species are of considerable economic importance due to their pathogenic effects on agriculture and livestock. Cephalosporins) |
Ceftriaxone
Ceftriaxone
A broad-spectrum cephalosporin antibiotic and cefotaxime derivative with a very long half-life and high penetrability to meninges, eyes and inner ears.
Cephalosporins 2 g every 12 hours OR Cefotaxime Cefotaxime Semisynthetic broad-spectrum cephalosporin. Cephalosporins 2 g every 4–6 hours |
21–28 days |
| Pseudomonas aeruginosa Pseudomonas aeruginosa A species of gram-negative, aerobic, rod-shaped bacteria commonly isolated from clinical specimens (wound, burn, and urinary tract infections). It is also found widely distributed in soil and water. P. Aeruginosa is a major agent of nosocomial infection. Pseudomonas |
Cefepime
Cefepime
A fourth-generation cephalosporin antibacterial agent that is used in the treatment of infections, including those of the abdomen, urinary tract, respiratory tract, and skin. It is effective against pseudomonas aeruginosa and may also be used in the empiric treatment of febrile neutropenia.
Cephalosporins 2 g every 8 hours OR Ceftazidime Ceftazidime Semisynthetic, broad-spectrum antibacterial derived from cephaloridine and used especially for pseudomonas and other gram-negative infections in debilitated patients. Cephalosporins 2 g every 8 hours OR Meropenem Meropenem A thienamycin derivative antibacterial agent that is more stable to renal dehydropeptidase I than imipenem, but does not need to be given with an enzyme inhibitor such as cilastatin. It is used in the treatment of bacterial infections, including infections in immunocompromised patients. Carbapenems and Aztreonam 2 g every 8 hours |
21 days |
| Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess(methicillin-susceptible) |
Nafcillin
Nafcillin
A semi-synthetic antibiotic related to penicillin.
Staphylococcal Scalded Skin Syndrome (SSSS) 2 g every 4 hours OR Oxacillin 2 g every 4 hours |
10–14 days |
| Staphylococcus aureus Staphylococcus aureus Potentially pathogenic bacteria found in nasal membranes, skin, hair follicles, and perineum of warm-blooded animals. They may cause a wide range of infections and intoxications. Brain Abscess(methicillin-resistant) and Staphylococcus epidermidis Staphylococcus epidermidis A species of staphylococcus that is a spherical, non-motile, gram-positive, chemoorganotrophic, facultative anaerobe. Mainly found on the skin and mucous membrane of warm-blooded animals, it can be primary pathogen or secondary invader. Staphylococcus |
Vancomycin
Vancomycin
Antibacterial obtained from streptomyces orientalis. It is a glycopeptide related to ristocetin that inhibits bacterial cell wall assembly and is toxic to kidneys and the inner ear.
Glycopeptidesa 15–20 mg/kg every 8–12 hours Consider adding rifampin Rifampin A semisynthetic antibiotic produced from streptomyces mediterranei. It has a broad antibacterial spectrum, including activity against several forms of Mycobacterium. In susceptible organisms it inhibits dna-dependent RNA polymerase activity by forming a stable complex with the enzyme. It thus suppresses the initiation of RNA synthesis. Rifampin is bactericidal, and acts on both intracellular and extracellular organisms. Epiglottitis 600 mg daily.d |
|
| Propionibacterium acnes Propionibacterium acnes A bacteria isolated from normal skin, intestinal contents, wounds, blood, pus, and soft tissue abscesses. It is a common contaminant of clinical specimens, presumably from the skin of patients or attendants. Acne Vulgaris | Penicillin Penicillin Rheumatic Fever G 4 million units every 4 hours | 10–14 days |
Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis:
Viral meningitis Viral meningitis Viral infections of the leptomeninges and subarachnoid space. Togaviridae infections; flaviviridae infections; rubella; bunyaviridae infections; orbivirus infections; picornaviridae infections; orthomyxoviridae infections; rhabdoviridae infections; arenaviridae infections; herpesviridae infections; adenoviridae infections; JC virus infections; and retroviridae infections may cause this form of meningitis. Clinical manifestations include fever, headache, neck pain, vomiting, photophobia, and signs of meningeal irritation. Meningitis is usually self-limiting Self-Limiting Meningitis in Children and requires only supportive management. Antiviral Antiviral Antivirals for Hepatitis B therapy is indicated only if viral encephalitis Viral encephalitis Inflammation of brain parenchymal tissue as a result of viral infection. Encephalitis may occur as primary or secondary manifestation of togaviridae infections; herpesviridae infections; adenoviridae infections; flaviviridae infections; bunyaviridae infections; picornaviridae infections; paramyxoviridae infections; orthomyxoviridae infections; retroviridae infections; and arenaviridae infections. Encephalitis is also suspected; in selected and/or severe cases.
Fungal meningitis Fungal meningitis Meningitis caused by fungal agents which may occur as opportunistic infections or arise in immunocompetent hosts. Meningitis:
Other types of meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis:
Vaccinations can protect against certain types of meningitis Meningitis Meningitis is inflammation of the meninges, the protective membranes of the brain, and spinal cord. The causes of meningitis are varied, with the most common being bacterial or viral infection. The classic presentation of meningitis is a triad of fever, altered mental status, and nuchal rigidity. Meningitis:
Routine vaccination Vaccination Vaccination is the administration of a substance to induce the immune system to develop protection against a disease. Unlike passive immunization, which involves the administration of pre-performed antibodies, active immunization constitutes the administration of a vaccine to stimulate the body to produce its own antibodies. Vaccination schedule:
Chemoprophylaxis Chemoprophylaxis Meningitis in Children:[11,15,17]