Jaundice is the abnormal yellowing of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions and/or sclera Sclera The white, opaque, fibrous, outer tunic of the eyeball, covering it entirely excepting the segment covered anteriorly by the cornea. It is essentially avascular but contains apertures for vessels, lymphatics, and nerves. Eye: Anatomy caused by the accumulation of bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism. Hyperbilirubinemia is caused by either an increase in bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism production or a decrease in the hepatic uptake, conjugation Conjugation A parasexual process in bacteria; algae; fungi; and ciliate eukaryota for achieving exchange of chromosome material during fusion of two cells. In bacteria, this is a unidirectional transfer of genetic material; in protozoa it is a bi-directional exchange. In algae and fungi, it is a form of sexual reproduction, with the union of male and female gametes. Bacteriology, or excretion of bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism. Etiologies often involve the liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy and can be prehepatic, intrahepatic, or posthepatic. Other symptoms of hyperbilirubinemia include pruritus Pruritus An intense itching sensation that produces the urge to rub or scratch the skin to obtain relief. Atopic Dermatitis (Eczema), pale stools, and darkened urine. The diagnosis is made based on liver function tests Liver function tests Liver function tests, also known as hepatic function panels, are one of the most commonly performed screening blood tests. Such tests are also used to detect, evaluate, and monitor acute and chronic liver diseases. Liver Function Tests and imaging. Management is focused on treatment of the underlying condition.
Last updated: Oct 13, 2022
Jaundice is caused by an elevation of serum bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism (hyperbilirubinemia), which can be caused by:
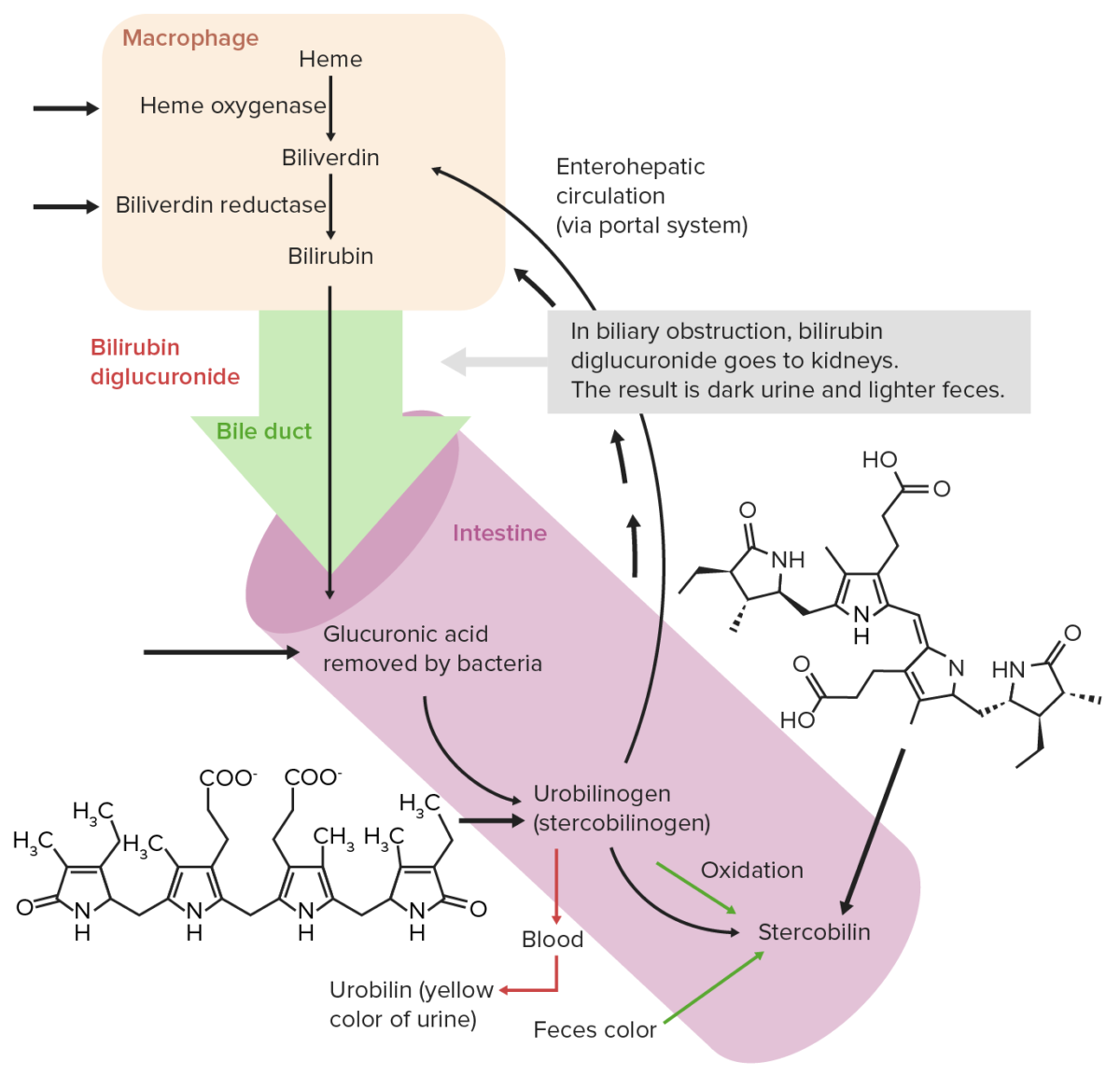
Normal extrahepatic circulation of bilirubin
Image by Lecturio. License: CC BY-NC-SA 4.0Common causes of hyperbilirubinemia can be remembered with the mnemonic HOT Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy:
Etiologies of jaundice can be broken down as conditions that cause either an elevation in indirect, direct, or mixed hyperbilirubinemia (see table below).
| Indirect (unconjugated) hyperbilirubinemia | Hemolytic disorders | Inherited:
|
|---|---|---|
| Ineffective erythropoiesis Erythropoiesis The production of red blood cells (erythrocytes). In humans, erythrocytes are produced by the yolk sac in the first trimester; by the liver in the second trimester; by the bone marrow in the third trimester and after birth. In normal individuals, the erythrocyte count in the peripheral blood remains relatively constant implying a balance between the rate of erythrocyte production and rate of destruction. Erythrocytes: Histology | Inherited:
|
|
| Increased bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism production | Secondary to:
|
|
| Decreased bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism conjugation Conjugation A parasexual process in bacteria; algae; fungi; and ciliate eukaryota for achieving exchange of chromosome material during fusion of two cells. In bacteria, this is a unidirectional transfer of genetic material; in protozoa it is a bi-directional exchange. In algae and fungi, it is a form of sexual reproduction, with the union of male and female gametes. Bacteriology |
|
|
| Drugs |
|
|
| Direct (conjugated) hyperbilirubinemia | Biliary tract Biliary tract Bile is secreted by hepatocytes into thin channels called canaliculi. These canaliculi lead into slightly larger interlobular bile ductules, which are part of the portal triads at the “corners” of hepatic lobules. The bile leaves the liver via the right and left hepatic ducts, which join together to form the common hepatic duct. Gallbladder and Biliary Tract: Anatomy obstruction | Secondary to:
|
| Biliary tract Biliary tract Bile is secreted by hepatocytes into thin channels called canaliculi. These canaliculi lead into slightly larger interlobular bile ductules, which are part of the portal triads at the “corners” of hepatic lobules. The bile leaves the liver via the right and left hepatic ducts, which join together to form the common hepatic duct. Gallbladder and Biliary Tract: Anatomy disease |
|
|
| Decreased excretion/reuptake of bilirubin Bilirubin A bile pigment that is a degradation product of heme. Heme Metabolism: |
|
|
| Mixed (both indirect and direct) hyperbilirubinemia | Chronic conditions |
|
Etiologies of jaundice can also be broken down based on the organ system (hepatic and cholestatic conditions).
Intrahepatic
Extrahepatic
These symptoms may be associated with:
Further workups are outlined in the image below.
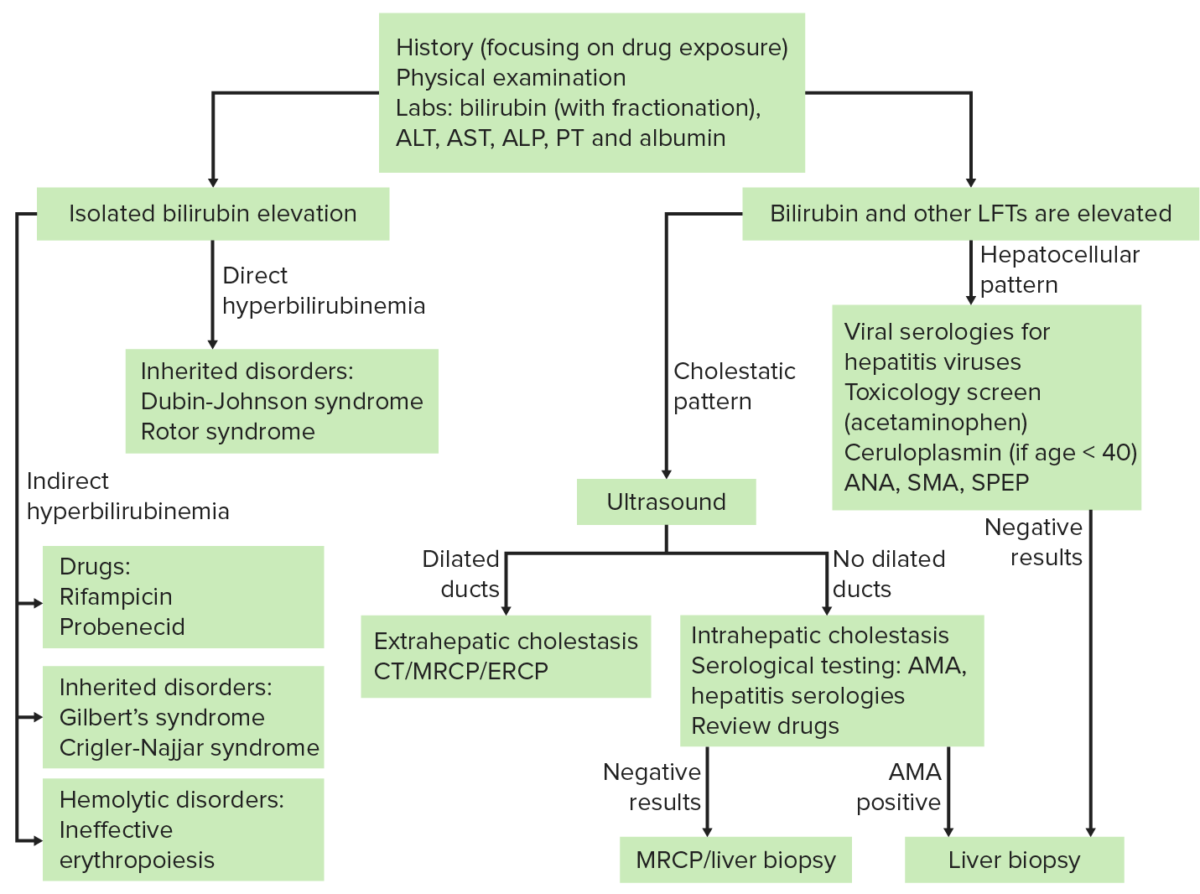
Key abbreviations:
ANA: antinuclear antibody
SMA: smooth-muscle antibody
SPEP: serum protein electrophoresis
AMA: antimitochondrial antibody
MRCP: magnetic resonance cholangiopancreatography
| Prehepatic | Intrahepatic | Posthepatic | ||
|---|---|---|---|---|
| Stool color | Dark | Pale, clay-colored | Pale, clay-colored | |
| Blood work | Indirect bilirubin Indirect Bilirubin Liver Function Tests | ↑↑ | ↑ | Normal |
| Direct bilirubin Direct bilirubin Liver Function Tests | Normal | ↑ | ↑↑ | |
| Anemia Anemia Anemia is a condition in which individuals have low Hb levels, which can arise from various causes. Anemia is accompanied by a reduced number of RBCs and may manifest with fatigue, shortness of breath, pallor, and weakness. Subtypes are classified by the size of RBCs, chronicity, and etiology. Anemia: Overview and Types | Present | Absent | Absent | |
| Alkaline phosphatase Alkaline Phosphatase An enzyme that catalyzes the conversion of an orthophosphoric monoester and water to an alcohol and orthophosphate. Osteosarcoma | Normal | ↑ | ↑↑ | |
| Transaminases Transaminases A subclass of enzymes of the transferase class that catalyze the transfer of an amino group from a donor (generally an amino acid) to an acceptor (generally a 2-keto acid). Most of these enzymes are pyridoxyl phosphate proteins. Autoimmune Hepatitis | Normal | ↑↑ | ↑ | |
| Urinalysis Urinalysis Examination of urine by chemical, physical, or microscopic means. Routine urinalysis usually includes performing chemical screening tests, determining specific gravity, observing any unusual color or odor, screening for bacteriuria, and examining the sediment microscopically. Urinary Tract Infections (UTIs) in Children | Color | Normal or dark | Dark | Dark or very dark |
| Urobilinogen Urobilinogen A colorless compound formed in the intestines by the reduction of bilirubin. Some is excreted in the feces where it is oxidized to urobilin. Some is reabsorbed and re-excreted in the bile as bilirubin. At times, it is re-excreted in the urine, where it may be later oxidized to urobilin. Heme Metabolism | ↑↑ | Normal or ↑ | Low or absent | |
| Bile Bile An emulsifying agent produced in the liver and secreted into the duodenum. Its composition includes bile acids and salts; cholesterol; and electrolytes. It aids digestion of fats in the duodenum. Gallbladder and Biliary Tract: Anatomy salt | Absent | Absent | Present | |

Jaundice: yellow discoloration of the skin due to bilirubin deposition
Image: “Jaundice08” by James Heilman, MD. License: CC BY 3.0
Scleral icterus: The first clinical sign of bilirubin deposition in the body.
Image: “Jaundice eye new” by CDC/Dr. Thomas F. Sellers/Emory University. License: Public DomainManagement is based on treatment of the underlying condition.
Pseudojaundice (carotenosis): yellow or orange discoloration of the skin Skin The skin, also referred to as the integumentary system, is the largest organ of the body. The skin is primarily composed of the epidermis (outer layer) and dermis (deep layer). The epidermis is primarily composed of keratinocytes that undergo rapid turnover, while the dermis contains dense layers of connective tissue. Skin: Structure and Functions caused by deposition of carotene. Can be distinguished from true jaundice because it does not cause discoloration of the conjunctival membranes of the sclerae. Usually secondary to excessive intake of substances rich in carotenoids Carotenoids The general name for a group of fat-soluble pigments found in green, yellow, and leafy vegetables, and yellow fruits. They are aliphatic hydrocarbons containing 4 terpene subunits. Leukoplakia (e.g., multivitamin supplements, oranges, carrots, apples, broccoli, papayas, kale).