Playlist
Show Playlist
Hide Playlist
Thyroiditis – Hyperthyroidism (Thyrotoxicosis)
-
Slides Hyperthyroidism incl. Graves Disease.pdf
-
Download Lecture Overview
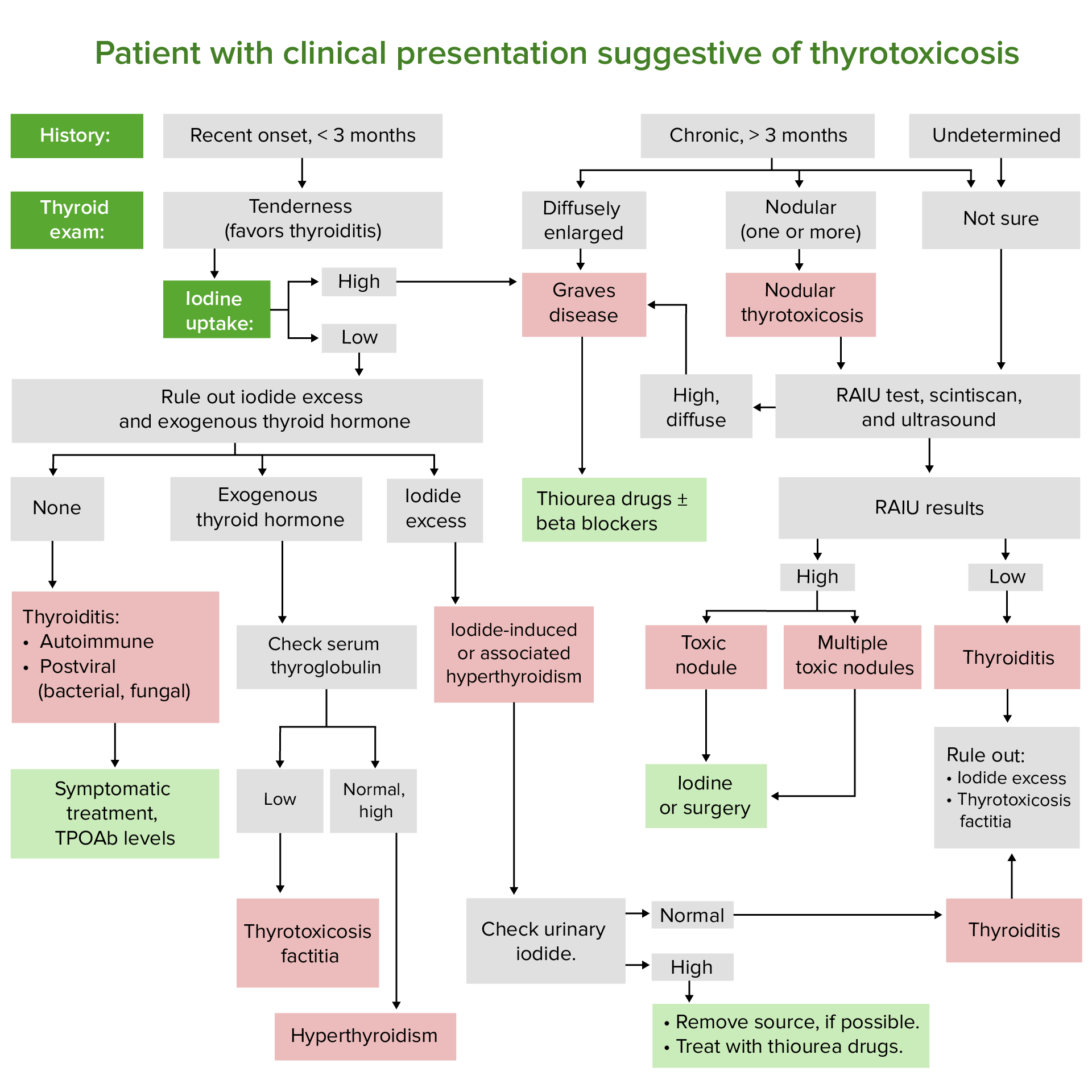
00:03 Let us now move on to thyroiditis with hyperthyroidism. 00:09 We’ve officially completed our discussion of Grave’s. 00:12 Let’s get into the group of diseases characterized by thyroid inflammation. 00:18 Chronic lymphocytic, the most common... 00:20 Now, this is interesting. 00:22 Hashimoto. 00:24 Hashimoto, most common cause of primary hypothyroidism in the US. 00:28 Hypothyroidism. 00:29 So, why is it under hyperthyroidism? Because of the following. 00:34 Whenever you have inflammation, -itis, inflammation of the thyroid, there’s every possibility that the colloid… Can you picture the colloid for me? The homogenous eosinophilic central region of your thyroid cell that stores your, harbours my thyroid hormones. 00:50 Any time there’s inflammation, that colloid “explodes”. 00:57 You may then release your T3, T4 into circulation in great quantity. 01:02 Welcome to thyroid storm. 01:04 There’s every possibility with any one of these thyroiditises that the patient may present initially with hyperthyroidism and that’s the topic that we’re sticking with here. 01:16 Do not ever forget that. 01:19 Chronic lymphocytic thyroiditis. 01:22 Acute bacterial (suppurative) thyroiditis – rare, but still possible. 01:27 Subacute thyroiditis. 01:29 What’s subacute mean? Slow, slow. 01:33 Subacute thyroiditis. 01:34 De Quervain, granulomatous thyroiditis. 01:38 Once again, destruction release of… Colloid releasing T3, T4 excessively. 01:46 Silent thyroiditis. 01:47 We’ll talk about this post-partum especially, with delivery. 01:51 We’ll see that coming up. 01:53 Amiodarone. 01:54 Amiodarone. 01:55 Take a look at the “iod” in amiodarone. 02:00 And doesn’t that resemble iodine? With amiodarone… You may be using this as an antiarrhythmic drug specifically and technically comes under class 3. 02:09 However, you know it has all classes of antiarrhythmic action. 02:14 Point is, the iodine, with amiodarone, some patients will respond with hyperthyroid type of presentation, whereas other patients may present with hypo. 02:25 I wish to be very clear here that the functioning or the side effect of amiodarone could either be hypo or hyper. 02:33 You really want to pay attention how is your patient presenting. 02:36 And we have what’s called Riedel’s thyroiditis. 02:40 Rare, but must know. 02:42 Let’s take a look at painful thyroiditis. 02:47 Infectious (suppurative) thyroiditis and deal with acute specifically. 02:52 Presents with abscess formation. 02:54 Thinking about bacteria. 02:56 Suppurative. 02:57 Gram-positive or gram-negative organism and gaining access most commonly and usually in children via fistula from the piriform sinus adjacent to the larynx, or via hematogenous spread in an immonucompromised patient. 03:13 So, if it’s a child, it would be through a fistula, through a sinus. 03:18 If it’s an adult, you’re thinking more about an immunocompromised patient. 03:22 Acute – rare, but still keep in mind. 03:25 A suppurative thyroiditis. 03:28 Painful. 03:29 Remember, if you have a bacterial infection, it’ll usually be painful lymphadenopathy and it may present as painful thyroiditis. 03:38 Acute. 03:40 Chronic. 03:42 Chronic thyroiditis usually caused by Aspergillus, Pneumocystis in immunocompromised patients that you’re quite familiar with. 03:50 Chronic thyroiditis. 03:52 Sudden (acute) onset of neck pain, usually unilateral with fever. 03:57 Well, behind your thyroid gland is oesophagus – may then constrict it, therefore result in obstruction, dysphagia. 04:06 And whenever you have bacterial infection, you expect it to be, or even any type of infection, leukocytosis. 04:14 Differential – haemorrhage into the thyroid nodule and subacute thyroiditis are your differentials that you want to keep in mind. 04:23 Continuing discussion of painful thyroiditis and here are some important differentials. 04:28 Management. 04:29 Ultra-sound. 04:31 Infectious thyroiditis – you would expect to find abscess. 04:33 So, therefore, you would expect to find a fluid-filled type of structure within the thyroid gland resulting in, or diagnosing your patient more or less with bacterial. 04:47 Whereas subacute thyroiditis, as a differential, diffusive heterogeneity and low intensity vascular flow. 04:56 So, diffuse heterogeneity, meaning to say that here on ultra-sound instead of finding a homogenous type of structure, it would be heterogeneous. 05:06 Diffuse subacute. 05:07 Then thyroid gland is going to be affected. 05:10 Abscess is localised in one region. 05:13 Acute. 05:14 Fine needle aspiration (FNA). 05:17 Infectious thyroiditis – fluid collection with microbes, so you want to see as to… You want to culture the organisms that you would expect to find within your perhaps abscess. 05:29 If it’s subacute, maybe. 05:31 Remember, this is more chronic in nature, so therefore you would expect to find more of a granulomatous type of inflammation, so therefore, you’d expect to find multinucleated giant cells. 05:42 Any type of granuloma. 05:44 Treatment – well, depends. 05:46 IV antibiotic and ultimately you’re thinking about draining your abscess. 05:51 Important points of properly managing a patient who’s presenting with hyperthyroidism, but is painful thyroiditis. 06:01 Acute, subacute, ultra-sound, FNA. 06:08 Painful thyroiditis – differentials. 06:10 Subacute. 06:11 We’ll put together granulomatous and DeQuervain thyroiditis, so this is much longer. 06:18 Usually here you’re not going to find bacterias much. 06:22 Acute – bacterial, abscess, ultra-sound, localised lesions that you’d find in your thyroid. 06:29 Subacute – viral infections: MUMPS, coxsackie. 06:34 Often preceding in upper respiratory tract infection, strongly associated with HLA-B35. 06:41 Limited, painful, tender. 06:46 More common in women. 06:48 Typically 3-6 weeks of pain and thyrotoxicosis. 06:51 What does that mean? Hyperthyroidism followed by several months of hypothyroidism and recovery is going to take place. 07:00 Now, let’s get into further continuum of thyroiditis. 07:03 It’s initially there might be destruction of colloid. 07:06 You might have increase of your T3, T4 and at some point things are going to slow down and upon recovery, because this is viral, may result in normal euthyroidic function. 07:21 Because it’s painful thyroiditis and you’re thinking about viral, you are thinking about symptomatic treatment and anti-inflammatories. 07:30 FNA – focal destruction of your thyroid tissues by granulomatous inflammation. 07:36 And what kind of cells are you going to find here? Good. 07:40 Multinucleated giant cells. 07:43 Clinical note – radiation thyroiditis may manifest 5-10 days. 07:47 You’re looking at approximately week post-radioiodine treatment of Grave’s disease. 07:53 So, even if you’re thinking about perhaps giving your patient radioactive iodine, there’s every possibility that may result in what’s known as radiation thyroiditis. 08:03 Keep that in mind. 08:04 I’d like to show you a graph here with the continuum of thyroiditis. 08:11 Up until this point, I’ve been talking to you about how you may destroy the colloid releasing T3, T4, but as the sequence takes place for thyroiditis, then what do you want to know? You can have a patient initially with hyperthyroidism. 08:26 Take a look at X-axis on the graph. 08:29 If it’s hyperthyroidism, you’d expect your T3, T4 to be high. 08:33 Take a look at the blue line. 08:34 And you find that to be elevated. 08:36 If you find your T3, T4 to be elevated, then if you are thinking about diagnosis radioactive iodine, which is the red line, when you have such T3, T4 elevated, what is your TSH level? It’s depressed. 08:53 Take a look at the green line, in specifically hyperthyroid segment. 08:58 Increased T3, T4, decreased TSH. 09:02 Welcome to thyroiditis. 09:04 Here, because of decreased TSH activity on the thyroid gland. 09:08 What about your radioactive iodine uptake? It is decreased, because you don’t have as much receptor activity. 09:15 Let’s continue. 09:16 Through thyroiditis, this is not Grave’s disease, this is not Hashimoto, even though Hashimoto could present a little bit like this. 09:26 This is thyroiditis, subacute. 09:29 Then you go through euthyroid phase. 09:30 So, what does that mean? Now, you have levels of your thyroid gland or thyroid receptors for your thyroid hormones which are decreasing. 09:39 As the thyroid hormone levels are decreasing, take a look at the blue line, then you would expect your TSH to be rising along with it. 09:47 You’d expect your radioactive iodine to also increase. 09:52 With continuous destruction of your thyroid gland, maybe because of viral infections, then you expect your thyroid hormones to depress even further so you get into your third segment on your X-axis, your hypothyroid. 10:07 Notice here, please, that your T3, T4 decreased. 10:11 Therefore, you would expect to find an increase in TSH and, thus, you expect increased activity of your TSH receptors and your radioactive iodine is being taken up in greater quantity. 10:26 Once the viral infection has been passed, then you go into a state of euthyroidism. 10:32 Welcome to recovery. 10:35 Notice now that at any point in time in a patient, so you’re looking at approximately 3-6 weeks of hyperthyroidism, maybe state of euthyroid, maybe state of hypo and then with the viral, you’d expect it to be recovery. 10:50 Obviously, such a thing would not be taking place with Hashimoto. 10:55 You will see. 10:59 Silent lymphocytic thyroiditis. 11:01 1-5% of your cases of hyperthyroidism. 11:05 Once again, release of your T3, T4. 11:08 Any woman non-post-partum or man a who’s had symptoms of mild hyperthyroidism for less than 2 months. 11:17 This is painless, silent, lymphocytic. 11:20 That’s short and has a small diffuse goiter and no thyroid enlargement. 11:25 That’s your definition of a painless, silent thyroiditis. 11:31 Autoimmune – could be a variant and could be a variant of what’s known as your Hashimoto, but in milder form. 11:38 Meds – interferon-?, interleukin-2, lithium – may also result in destruction of your thyroid; may present as silent, painless thyroiditis. 11:49 Phasic course similar to subacute – what does that mean to you? Meaning to say that you would be in a state of hyperthyroidism, maybe euthyroid and unfortunately 25% of your patient may actually remain hypothyroid permanently. 12:03 Post-partum, so, now, a pregnant woman is giving delivery. 12:08 Thyroiditis occurs within one year after parturition or after spontaneous or induced abortion. 12:17 Patient may present with, once again, hyperthyroid, euthyroid, hypothyroid. 12:24 Similar clinical pathogenetically to painless thyroiditis. 12:28 However, differs from painless thyroiditis in that more patients have elevated levels of serum anti-thyroid antibody or anti-, let’s say thyroglobulin, or anti-thyroid peroxidise; TPO stands for thyroid peroxidise, increasing likelihood of permanent thyroid disease later. 12:48 So, couple of things that you want to keep in mind here as you walk through your painless thyroiditis is, well, similarly talk about post-partum thyroiditis. 12:59 However, along with this, there might be issues with autoimmune, meaning to say they were referring to our Hashimoto perhaps.
About the Lecture
The lecture Thyroiditis – Hyperthyroidism (Thyrotoxicosis) by Carlo Raj, MD is from the course Thyroid Gland Disorders.
Included Quiz Questions
What is considered a variant of Hashimoto thyroiditis?
- Silent thyroiditis
- de Quervain thyroiditis
- Acute bacterial thyroiditis
- Riedel thyroiditis
- Amiodarone induced thyroiditis
What is the most common origin of infection in children presenting with acute suppurative thyroiditis?
- Fistula from piriform sinus
- Underlying TB infection
- Hematogenous spread
- Aspergillus
- Pneumocystis
On fine-needle aspiration, a patient was found to have multinucleated giant cell granulomas. What is the most likely diagnosis?
- de Quervain thyroiditis
- Suppurative thyroiditis
- Amiodarone-induced thyroiditis
- Silent thyroiditis
- Riedel thyroiditis
What is FALSE regarding granulomatous thyroiditis?
- Treatment includes IV antibiotics.
- It is strongly associated with HLA-B35.
- It is associated with mumps and coxsackie viruses.
- It features a period of thyrotoxicosis followed by hypothyroidism.
- Focal destruction of thyroid tissue occurs.
How does postpartum painless thyroiditis differ from non-postpartum painless thyroiditis?
- More patients have elevated levels of serum antithyroid antibodies.
- Diffuse goiter
- Autoimmune etiology
- Mild hyperthyroidism
- Painless
What is NOT associated with silent thyroiditis?
- Glucocorticoids
- Pregnancy
- IFN-alpha
- IL-2
- Lithium
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |