Playlist
Show Playlist
Hide Playlist
Secondary Dilated Cardiomyopathy – Cardiomyopathy
-
Slides 05 Cardiology Alpert.pdf
-
Download Lecture Overview
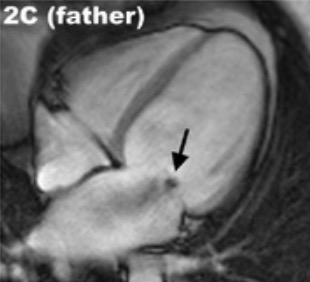
00:01 of heart failure particularly related to cardiomyopathy as a very malignant disease within cardiology. 00:01 Ischemic cardiomyopathy, along with hypertrophic cardiomyopathy, are the two commonest forms of cardiomyopathy seen. In the dilated cardiomyopathy due to ischemic heart disease, very often the patients will have had symptomatic myocardial infarcts, usually multiples, and each one of these damages the left ventricle with the end result that one ends up with markedly reduced left ventricular muscle and a dilated cardiomyopathy. Something that we don’t understand is that some patients show up for the first time with heart failure, never having had a clinical heart attack or myocardial infarct, never having had angina, and yet when we do their coronary angiogram as part of the evaluation, we discover terrible, severe, advanced coronary disease as the cause. Why these patients have no symptoms and other patients have clear-cut symptoms is still a mystery and is the subject of intense investigation. 00:52 Hypertension, untreated, can also lead to dilated cardiomyopathy by putting a major stress on the left ventricle that eventually causes it to fail and dilate. Valvular heart disease, longstanding mitral regurgitation, longstanding aortic regurgitation, untreated, also eventually can lead to a dilated cardiomyopathy. The next one listed on your list here, the anthracyclines, these are drugs used in a variety of cancers, but particularly for breast cancer, particularly metastatic breast cancer, and they can cause heart damage. And so, the cardiologists are often involved with the oncologist in carefully monitoring the patient who’s receiving these drugs and we stop the treatment as soon as we start to see some heart injury. There’s a small number of women who, following pregnancy, will develop a dilated cardiomyopathy. Again, there seems to be a genetic predisposition here. And finally, chronic, heavy use of alcohol leads to a dilated cardiomyopathy, among other problems. Now, let’s talk a little bit about ischemic dilated cardiomyopathy because again, this is a very very common form. It seems that this is the most common form of dilated cardiomyopathy, although the genetic forms now compete with it for most common status. It’s, as we’ve talked about, caused by repeated injuries from ischemia that can be symptomatic or asymptomatic. And, in fact, many of these patients come first to attention when they have a myocardial infarction that is symptomatic. But others, as I’ve told you, come to attention when they’ve never had any symptoms and we discover, to our surprise, that the patient has severe coronary artery disease. The prognosis is not good with the dilated cardiomyopathy, as I’ve been expressing throughout this section. 02:47 Any form of dilated cardiomyopathy has a poor prognosis. The ischemic form has the worst prognosis. Now, let’s talk for a few moments about diagnosis. We would, of course, love to diagnose these patients early in the course of their cardiomyopathy. Unfortunately, they usually come to our attention when they develop symptoms of quite significant heart failure. And, of course, in the heart failure segment, we’ve already talked about that. Patients may be short of breath. They may have peripheral swelling and edema. Sometimes the ischemic form, the patient will have had some ischemic event, and then when we do the echocardiogram and the catheterization, we discover, to our surprise, that the left ventricle has been severely injured, has a markedly reduced ejection fraction that is a reduced percentage of blood that it squeezes out with each beat. There are often electrical abnormalities, both atrial and ventricular arrhythmias. We’re going to talk about the arrhythmias in a few moments. And, of course, there are enla-, there’s enlargement on the electrocardiogram of the left atrium and also, often evidence for enlargement of the left ventricle as well. On physical exam, it’s the heart failure exam. The heart may feel enlarged when you feel the chest. There is often a third heart sound which is a sign that the ventricle has been severely damaged. There may be sounds in the lung that suggest fluid. There may be edema in the legs, as I’ve already said. 04:25 And one may even have, as I mentioned before, mitral or tricuspid regurgitation murmurs from stretching of the valve annulus or ring in which the valve is contained. The workup for the diagnosis usually starts, of course, with the physical exam and a history, followed by an electrocardiogram. Usually, by then, we’re starting to have a clue because we see it's a heart failure patient, that we’re dealing with a dilated cardiomyopathy. 04:52 And then the echocardiogram shows us the picture that really confirms it. We usually do a coronary angiogram to distinguish the ischemic form from the forms that are not ischemic, for example, the genetic or alcoholic ones or other etiologies. Occasionally, we’ll do a magnetic resonance image because it gives us an idea about what is the underlying structure of the myocardium. There might be a clue, “Oh, this is ischemic,” or “No, this is secondary to a chemical that’s being used for treatment of cancer,” or could be from alcohol. These days, we’re doing more MRIs because they give us a lot of information about the structure of the myocardium in patients with dilated cardiomyopathy. And again, coronary angiography to make sure we’re not dealing with ischemic cardiomyopathy. In some, not very many, individuals with dilated cardiomyopathy, when we do coronary bypass and give new blood flow to the heart muscle, some of the heart muscle recovers. And so, there’s partial recovery of the ischemic cardiomyopathic patient, but usually, that doesn’t happen. Usually, the ventricle is too damaged and scarred to recover and after medical therapy fails to work, these patients are often candidates for heart transplant. But, we’ll talk about that in a few minutes. So, the therapy, of course, is the same therapy we talked about for heart failure. Beta Blockers often improve the situation by decreasing the work of the heart. ACE inhibitors or angiotensin receptor blockers that block the renin-angiotensin system, decrease the blood pressure, improve vascular function and often help. Sometimes the patients need small and sometimes large doses of diuretics and sometimes these are combined with mineralocorticoid diuretics such as Aldactone that help to decrease the edema tendency in these patients. We, of course, try and reduce salt in their diet. Sometimes regular exercise helps. We have to pay attention to electrical abnormalities - arrhythmias. 07:04 And in a small number of patients, sometimes a special pacemaker can re-coordinate the electrical activation of the ventricle and improve the contractility a bit. So, there’s a whole variety of therapies usually starting with drugs and watching out how much sodium is in the diet and some exercise and then progressing to more aggressive things, special pacemaker therapies and finally heart transplant in the end. 07:32 Hypertrophic cardiomyopathy is the other very common form of cardiomyopathy in the population. 07:38 It occurs in about a hundred out of a hundred thousand people, and as I’ve said before, most of these individuals have the disease in a completely benign form. They live long lives and they have no problems. The disease is genetic. It’s an autosomal-dominant inheritance and there have now been discovered more than 1,000 different mutations that lead to hypertrophic cardiomyopathy. What happens is that the heart muscle cells develop in an abnormal fashion so that instead of being lined up and parallel, they are in a random order and they pull against each other in abnormal fashion so that there is a marked tendency for individual cells to hypertrophy that is to increase in size and volume and this, of course, then results eventually in a marked increase in size and volume of the left ventricle. There are a variety of different forms of hypertrophic cardiomyopathy. The commonest one involves marked hypertrophy of the septum, but there can be forms in which the apex is hypertrophied, the base is hypertrophied, and even, sometimes, the hypertrophy extends into the right ventricle. 08:48 When the disease was first described in the 1960s, it was thought to be a horrible thing. 08:52 Why? Because we only saw patients who were hospitalized with complications. Well, about 20 years ago, the Italians did a whole community survey where they went into a community and they did echocardiograms on everybody in the community. And what they discovered was large numbers of patients with hypertrophic cardiomyopathy who were living normal lives... expectancies, who got to old age and in fact, I’ve seen patients well into their 90s with hypertrophic cardiomyopathy. It turns out the vast majority of patients with hypertrophic cardiomyopathy do just fine. However, there is a small sub-group that has malignant ventricular arrhythmias and as I said before, the commonest cause of death in young athletes who are involved in sports, particularly in high-competition sports - basketball, football, soccer and so forth. These individuals can develop malignant arrhythmias and have cardiac arrest on the playing field. Again, genetic disease, quite common, but in the main, quite benign. And here you see some statistics for how common in the population. Not that common, certainly nowhere near as common as coronary artery disease, but nevertheless, more common, a little more common, than the dilated cardiomyopathy, at least in some series. Although in other series, the two are almost equivalent. So, let’s take a look again at the genetic underlying factor. I think I told you already, it has to do with abnormalities in the DNA that lead to abnormalities in the contraction machinery of the heart and that there’s a thousand different mutations that lead to this disease. And there’s a variety of forms and we’ll take a little look at that. All right, so here’s a diagram. Again, the
About the Lecture
The lecture Secondary Dilated Cardiomyopathy – Cardiomyopathy by Joseph Alpert, MD is from the course Cardiac Diseases.
Included Quiz Questions
Which of the following findings is less likely in a patient with ischemic dilated cardiomyopathy without significant obstructive valvulopathy?
- High-pitched murmur in the base of the heart radiating to the carotids
- A narrow pulse pressure
- 3ʳᵈ heart sound
- Enlarged and displaced apex beat
- 4th heart sound
Which of the following drugs is most likely to cause dilated cardiomyopathy at therapeutic levels?
- Doxorubicin
- Propranolol
- Levothyroxine
- Prednisone
Which of the following is not a treatment option for dilated cardiomyopathy?
- Pericardiectomy
- Ventricular assist device
- Cardiac transplantation
- Angiotensin-converting enzyme inhibitors
- Furosemide
Customer reviews
3,6 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
1 |
| 1 Star |
|
1 |
Very good concepts are explained in these lectures. Classification is explained well in the first lecture with a flow diagram.
The topic it's well explained, clear and highly related to previous lectures.
mixed information,make me lost.i need to read another reference to understand this confusion
Good lecture. dont understand why someone gave it only a one