A 70-year-old Caucasian woman presents with a 2-week history of blood-tinged sputum. Her past medical history is significant for peptic ulcer disease for which she underwent triple-drug therapy. She is a lifetime non-smoker and worked as a teacher before retiring at the age of 60 years. A review of systems is significant for a weight loss of 6.8 kg (15 lb) over the last 5 months. Her vitals include: blood pressure 135/85 mm Hg, temperature 37.7°C (99.9°F), pulse 95/min, and respiratory rate 18/min. Physical examination is unremarkable. A contrast CT scan of the chest shows an irregular mass in the peripheral region of the inferior lobe of the right lung. A CT-guided biopsy is performed and reveals malignant tissue architecture and gland formation with a significant amount of mucus. Which of the following is the most significant risk factor for this patient’s most likely diagnosis?
A. Medications
B. Occupational history
C. Past medical history
D. Race
E. Sex
A 47-year-old woman presents to her physician for difficulty swallowing. She states that she intentionally delayed seeing a physician for this issue. She says her primary issue with swallowing is that her mouth always feels dry so she has difficulty chewing food to the point that it can be swallowed. On physical examination, her oral mucosa appears dry. Both of her eyes also appear dry. Several enlarged lymph nodes are palpated. Which of the following patterns of reactive lymphadenitis is most commonly associated with this patient’s presentation?
A. Sinus hyperplasia
B. Follicular hyperplasia
C. Paracortical hyperplasia
D. Diffuse hyperplasia
E. Mixed B and T cell hyperplasia
A 35-year-old man is brought to the emergency room after he was found to have a blood pressure of 180/100 mm Hg during a routine health check-up with his family physician. Past medical history is insignificant and both of his parents are healthy. He currently does not take any medication. The patient’s blood pressure normalizes before the emergency department physician can evaluate him. During the physical examination, his blood pressure is 148/80 mm Hg, the heart rate is 65/min, the temperature is 36.8°C (98.2°F), and the respirations are 14/min. He has a round face, centripetal obesity, and striae on the skin with atrophy over the abdomen and thighs. On visual field examination, he is found to have a loss of vision in the lateral visual fields bilaterally. You order a low dose dexamethasone suppression test, which is positive. A high-dose dexamethasone suppression test is also conducted to measure ACTH. If the findings suggest a possible pituitary gland disorder, which of the following laboratory abnormalities is most likely in this patient?
A. Before test: ACTH high, after test: aldosterone suppression
B. Before test: ACTH low, after test: cortisol elevation
C. Before test: ACTH high, after test: cortisol suppression
D. Before test: ACTH low, after test: aldosterone normalizes
E. Before test: ACTH high, after test: cortisol elevation
A 28-year-old woman presents to the clinic with complaints of occasional low-grade fever and joint pain for 1 month. She also complains of morning stiffness in the proximal interphalangeal joints of both hands, which lasts for 5 to 10 minutes. She recently noticed a pink rash on her nose and cheekbones. Her family history is significant for similar complaints in her mother. She is not taking any medications. On examination, her temperature is 37.6°C (99.6°F), pulse is 74/min, blood pressure is 110/70 mm Hg, and respirations are 18/min. Aphthous ulcers are noted on her oral mucosa. Which of the following tests would be most specific for confirming the diagnosis in this patient?
A. Anti-double stranded DNA (dsDNA) antibodies
B. Anti-histone antibodies
C. Anti-topoisomerase (anti-Scl 70) antibodies
D. Anti-Ro antibodies
E. Antinuclear antibodies (ANA)
A 67-year-old woman presents to the clinic complaining of progressive fatigue over the past 4 months. She noticed that she is feeling increasingly short of breath after walking the same distance from the bus stop to her home. She denies chest pain, syncope, lower extremity edema, or a cough. She denies difficulty breathing while sitting comfortably, but she has increased dyspnea upon walking or other mildly strenuous activity. Her past medical history includes mild osteoporosis and occasional gastric reflux disease. She takes oral omeprazole as needed and a daily baby aspirin. The patient is a retired accountant and denies smoking history, but she does admit to 1 small glass of red wine daily for the past 5 years. Her diet consists of a Mediterranean diet that includes fruits, vegetables, and fish. She states that she has been very healthy previously, and managed her own health without a physician for the past 20 years. On physical examination, she has a blood pressure of 128/72 mm Hg, a pulse of 87/min, and an oxygen saturation of 94% on room air. HEENT examination demonstrates mild conjunctival pallor. Lung and abdominal examinations are within normal limits. Heart examination reveals a 2/6 systolic murmur at the right upper sternal border. The following laboratory values are obtained:
| Hematocrit | 29% |
| Hemoglobin | 9.8 mg/dL |
| Mean red blood cell volume | 78 fL |
| Platelets | 240,000/mm3 |
| White blood cells | 6,000/mm3 |
What is the most likely reticulocyte range for this patient?
A. < 1%
B. 0%
C. > 1.5%
D. > 5%
E. > 7%
A 5-year-old boy is brought to the office by his mother with complaints of facial puffiness and ‘frothy’ urine for 4 days. The puffiness first started in his eyes and then spread to the face. His mother does not provide any history of similar symptoms in the past. Past medical history is non-significant. His birth history is uneventful and all his vaccinations are up to date. The vital signs include: blood pressure 100/62 mm Hg, pulse 110/min, temperature 36.7°C (98.0°F), and respiratory rate 16/min. On examination, there is pitting edema of the upper and lower extremities bilaterally. Urinalysis results are as follows:
| pH | 6.2 |
| Color | Light yellow |
| RBC | None |
| WBC | 3–4/HPF |
| Protein | 4+ |
| Cast | Fat globules |
| Glucose | Absent |
| Crystal | None |
| Ketone | Absent |
| Nitrite | Absent |
| 24-hour urine protein excretion | 4.1 g |
A renal biopsy is sent which shows normal glomeruli on light microscopy. Which of the following is the most likely diagnosis?
A. Membranoproliferative glomerulonephritis
B. Post-infectious glomerulonephritis
C. Focal segmental glomerulosclerosis
D. Lipoid nephrosis
E. Membranous nephropathy
A 71-year-old woman with a past medical history of type 2 diabetes, hypercholesterolemia, and hypertension was admitted to the hospital 8 hours ago with substernal chest pain for management of acute non-ST-elevated myocardial infarction. ECG findings noted ST depressions and T wave inversions on anterolateral leads, accompanied by elevated cardiac enzymes.
Upon diagnosis, management with inhaled oxygen therapy, beta-blockers and aspirin, and low-molecular-weight heparin therapy were initiated, and the patient was placed on bed rest with continuous electrocardiographic monitoring. Since admission, she required 2 doses of sublingual nitric oxide for recurrent angina, and repeat troponin levels continued to rise. Given the patient’s risk factors, plans were made for early coronary angiography.
The telemetry nurse calls the on-call physician because she is concerned about the patient’s mild confusion and increasing need for supplemental oxygen. At bedside evaluation, vital signs include: heart rate is 122/min, blood pressure is 89/40 mm Hg, and pulse oximetry is 91% on 6L of oxygen by nasal cannula. Telemetry and a repeat ECG show sinus tachycardia.
The patient is breathing rapidly, appears confused, and complains of shortness of breath. On physical examination, the skin is cool and clammy. and appears pale and dull. She has diffuse bilateral pulmonary crackles, and an S3 gallop is noted on chest auscultation with no new murmurs. She has jugular venous distention to the jawline, rapid and faint radial pulses, and 1+ dependent edema. She is immediately transferred to the intensive care unit for respiratory support and precautions for airway security. Bedside sonography shows abnormal hypodynamic anterior wall movement and an ejection fraction of 20%, but no evidence of mitral regurgitation or ventricular shunt. Chest X-ray demonstrates cephalization of pulmonary veins and pulmonary edema. What is the most appropriate next step in the stabilization of this patient?
A. Insert two large-bore intravenous catheters and start rapid fluid resuscitation
B. Initiate dopamine therapy and diuresis
C. Start intravenous fluids and epinephrine therapy
D. Obtain blood cultures and start preliminary broad-spectrum antibiotics
E. Intubate the patient and perform an emergency cardiocentesis
A 49-year-old healthy woman presents to the outpatient department with swelling of the neck. Family history is negative for any thyroid disorders. Physical examination shows a nontender thyroid gland with a nodule on the right side. The thyroid gland is mobile on deglutition. Cervical lymphadenopathy is present. Fine-needle aspiration and cytology results show empty-appearing nuclei with central clearing, nuclear grooves, and branching structures interspersed with calcific bodies. Which of the following is the most likely diagnosis in this patient?
A. Follicular carcinoma
B. Papillary carcinoma
C. Medullary carcinoma
D. Anaplastic carcinoma
E. Follicular adenoma
A 3-day-old infant presents because the patient’s parents noticed that his skin was becoming yellow. The mother said that the patient eats well and has normal stools and urine color. He is her 1st child from a healthy pregnancy. The patient was born on time and delivered via spontaneous vaginal delivery with no complications. Family history is significant for a maternal aunt who died as an infant of unknown causes. The patient is afebrile and the vital signs are within normal limits. On physical examination, he is awake, calm, and appears healthy, except for the yellow tone of the skin and scleral icterus. Laboratory findings are significant for elevated unconjugated bilirubin, with a normal complete blood count. Other routine laboratory blood tests are within normal limits. The patient is treated with phototherapy, but his jaundice worsens and his unconjugated hyperbilirubinemia persists well into the 2nd week of life. Which of the following is the most likely diagnosis in this patient?
A. Crigler-Najjar syndrome type 2
B. Crigler-Najjar syndrome type 1
C. Hemolytic anemia
D. Gilbert syndrome
E. Neonatal jaundice
A 38-year-old man presents with pruritus and jaundice. Past medical history is significant for ulcerative colitis diagnosed 2 years ago and well-managed medically. He is vaccinated against hepatitis A and B and denies any recent travel abroad. The vital signs include blood pressure 118/76 mm Hg, heart rate 74/min, and respiratory rate 14/min. On physical examination, prominent hepatosplenomegaly is noted along with moderate right upper quadrant tenderness to palpation. Which of the following would confirm the most likely diagnosis in this patient?
A. Endoscopic retrograde cholangiopancreatography (ERCP)
B. Contrast CT of the abdomen
C. Ultrasound of the abdomen
D. Percutaneous liver biopsy
E. Magnetic resonance cholangiopancreatography (MRCP)
A 30-year-old man with a BMI of 33.7 kg/m2 presents with severe pain in his right toe that began this morning. He had a few beers last night at a friend’s party but otherwise has had no recent dietary changes. On examination, the right toe appears swollen, warm, red, and tender to touch. Joint aspiration is performed. What will examination of the fluid most likely reveal?
A. Increased glucose
B. Needle-shaped, negatively birefringent crystals on polarized light
C. Rhomboid-shaped, positively birefringent crystals on polarized light
D. Gram-negative diplococci
E. Anti-CCP antibodies
A 49-year-old woman presents to her physician with complaints of breast swelling and redness of the skin over her right breast for the past 1 month. She also mentions that the skin above her right breast appears to have thickened. She denies any pain or nipple discharge. The past medical history is significant for a total abdominal hysterectomy at 45 years of age. Results of her last mammogram 1 year ago were negative for any pathologic changes. On examination, the right breast is diffusely erythematous with gross edema and tenderness and appears larger than the left breast. The right nipple is retracted, and the right breast is warmer than the left breast. No localized mass is palpated. Which of the following statements best describes the patient’s most likely condition?
A. It is a benign lesion.
B. The inflammation is due to obstruction of dermal lymphatic vessels.
C. The lesion expresses receptors for estrogen and progesterone.
D. The lesion is due to streptococcal infection.
E. It shows predominant lymphatic spread.
A 22-year-old professional softball player is undergoing an annual check-up. Her medical history is significant for hallux valgus and scoliosis. She additionally notes that she frequently has bumps and bruises from playing softball, but she has no injuries today. Her family history is significant for heart disease. The patient’s blood pressure is 110/70 mm Hg, heart rate is 78/min, and respiratory rate is 15/min. A physical examination is unremarkable except for an indurated palpable mass on her left breast. A biopsy of the mass is performed. Which biopsy findings are most likely to be present in this patient?
A. Chronic inflammation with plasma cells
B. Necrotic fat with calcifications and giant cells
C. Leaf-like projections
D. Duct-like structures
E. Abundant extracellular mucin
A 40-year-old pregnant woman presents to the clinic in her 12th week of gestation. She does not have any complaints during this visit but comes to discuss her laboratory reports from her last visit. Her blood test results are within normal limits, but the abdominal ultrasound reports nuchal thickening with a septated cystic hygroma. Chorionic villus sampling is performed for a suspected chromosomal anomaly. Which of the following features can be expected to be present at the time of the birth of this fetus?
A. Congenital lymphedema of the hands and feet
B. Anal atresia
C. Port-wine stain on the forehead
D. Microphthalmia
E. Pectus carinatum
A 7-year-old boy comes to the clinic with his mother due to sudden puffiness of the eyes. The mother also is concerned about his abdominal distention, which she first noticed 5 days ago. The patient has no history of a recent infection in the upper respiratory tract, decreased urination, or gross hematuria. His vaccinations are up to date. His vitals include heart rate 86 beats per minute, respiratory rate 16 breaths per minute, temperature 37.6°C (99.7°F), and blood pressure 100/70 mm Hg. Physical examination reveals periorbital edema and abdominal distention with a fluid thrill. Laboratory findings include the following:
| Urinalysis | |
| Protein | 4+ |
| Urinary protein | 4 g/L |
| Creatinine ratio | 2.6 |
| Red blood cells | Nil |
| White blood cells | Nil |
| Urinary casts | Fatty casts |
| Serum creatinine | 0.4 mg/dL |
| > Serum albumin | 1.9 g/dL |
| Serum cholesterol | 350 mg/dL |
Ultrasonogram of the abdomen reveals kidneys with normal morphology and gross ascites. Which of the following statements best describes the complications this boy may develop?
A. Spontaneous bacterial peritonitis caused by Haemophilus influenzae
B. Urinary loss of calcium leading to hypocalcemia
C. Thromboembolism, requiring prophylactic anticoagulation
D. Acute renal failure due to intrinsic renal failure
E. Microcytic hypochromic anemia responding poorly to oral iron therapy
A 32-year-old woman presents to her primary care provider complaining of a psoriatic flare that has worsened over the past 2 days. The patient states that her psoriasis is normally well controlled. She also complains of some fatigue and states that she has recently developed pain and tenderness in the joints of her hands, with the right hand being more tender than the left. Her hands are stiff in the morning, and sometimes her fingers swell up. She attributes these changes to her new job, where she constantly uses her hands to manufacture cabinets. Physical examination reveals plaques with silvery scale on her elbows and knees. The distal joints of her right hand are mildly swollen, and the nails on both hands appear pitted. What is the most likely pathogenesis of her joint pain?
A. Local invasive infection of the joint space
B. Repetitive injury
C. Autoantibodies to the Fc portion of IgG
D. Deposition of crystals in the joint space
E. Release of TNF and activation of the RANKL pathway
A 45-year-old woman presents to the office with a chief complaint of a cough that has persisted for a month and a half. She also has night fevers and has lost 5 kg (11 lb) in the last 2 months. She recently returned from a 6-month trip to Peru. Her vitals include: heart rate 82/min, respiratory rate 17/min, temperature 38.0°C (100.4°F), and blood pressure 107/80 mm Hg. On auscultation, she has diminished respiratory sounds at the base of the right lung. Chest radiography shows an opacity in the right apex. What is the most likely cause of her presentation?
A. Echinococcosis
B. Tuberculosis
C. Pulmonary thromboembolism
D. Heart failure
E. Lung cancer
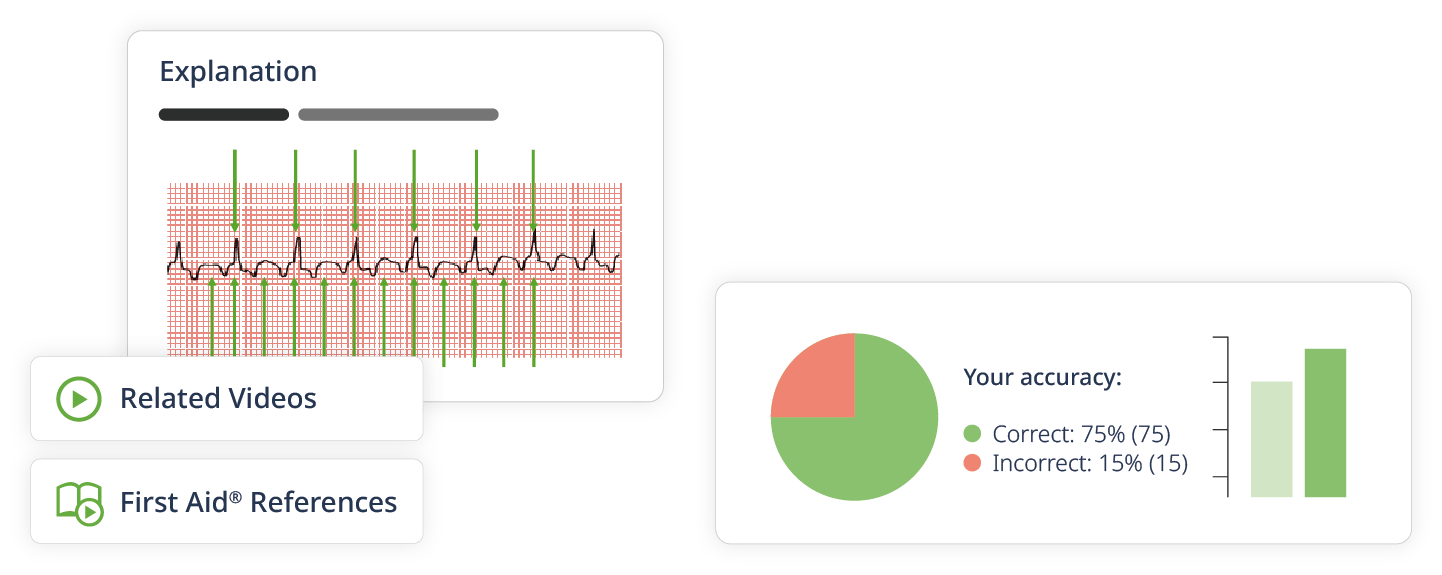
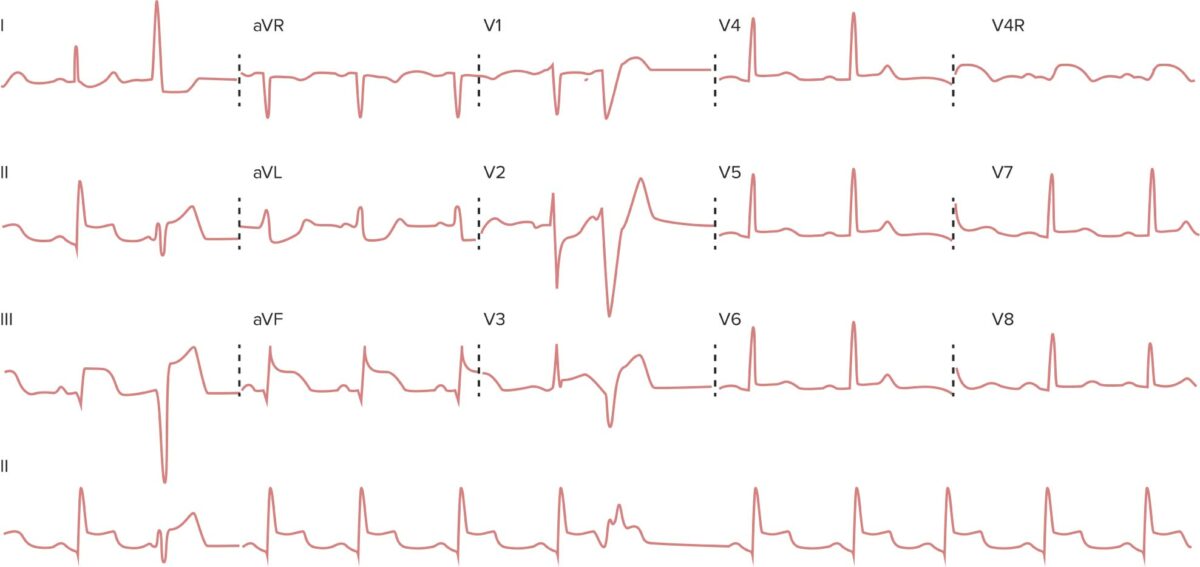
A 73-year-old woman arrives at the emergency department due to an intense central chest pain for 30 minutes this morning. She says the pain was cramping in nature and radiated down her left arm. She has a history of atrial fibrillation and type 2 diabetes mellitus. The vital signs include: pulse 98/min, respiratory rate 19/min, temperature 36.8°C (98.2°F), and blood pressure 160/91 mm Hg. Cardiovascular examination shows no abnormalities. Electrocardiogram (ECG) is shown below. Which of the following biochemical measures is most specific and would remain elevated for a week after this acute event?
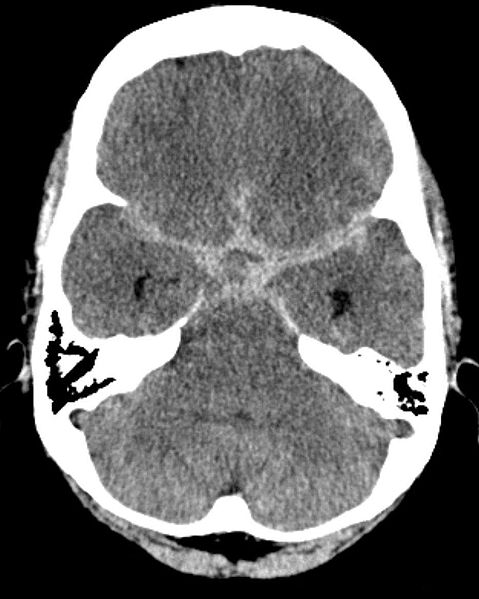
A 48-year-old woman presents with a sudden-onset severe headache that she describes as the worst in her life, followed by binocular horizontal diplopia and ptosis. Her past medical history is significant for hypertension. On admission, her vital signs include: blood pressure 130/70 mm Hg, heart rate 78/min, respiratory rate 18/min, and temperature 36.5°C (97.7°F). On neurological examination, the left eye deviates inferolaterally. There is also ptosis, mydriasis, and an absent pupillary light response on the left. A non-contrast CT of the head is performed and is shown below. Which of the following structures is most likely to be abnormal in this patient?
A. Cavernous segment of the internal carotid artery
B. Anterior communicating artery (ACom)
C. Posterior communicating artery (PCom)
D. Middle cerebral artery (MCA)
E. Pericallosal artery
A 40-year-old woman presents to her family physician with a 3-week history of swollen neck. The small, round, and painless swelling, which was detected 3 weeks ago in the middle of her neck, has now increased in size. The swelling is associated with sweaty palms and soles, insomnia, irritability, nervousness, and fatigue; however, the patient does not complain of fever, cervical lymphadenopathy, weight loss, vision problems, or body swelling. The patient’s medical history is negative for similar symptoms or a thyroid disorder. The vital signs are within normal limits. Local examination reveals a 3 x 3 cm round, non-tender, non-fluctuant, and non-pulsatile swelling in the anterior triangle of her neck. The patient carries a total white blood cell count of 10,200/mm3, including 70% neutrophils, 30% lymphocytes, and zero eosinophils.The erythrocyte sedimentation rate is 20 mm/hr (normal, 0–29 mm/hr). What is the most likely diagnosis?
A. Graves’ disease
B. De Quervain’s thyroiditis
C. Silent thyroiditis
D. Hashimoto’s thyroiditis
E. Riedel’s thyroiditis
Do you want to practice more Pathology questions?
Create a free Lecturio account and you’ll have access to the Lecturio question bank with more than 2,200 USMLE Step 1 practice questions.