Playlist
Show Playlist
Hide Playlist
Pulmonary Hypertension Medication – Drugs in Hypertension
-
Slides Pulmonary Hypertension Medication Drugs in Hypertension.pdf
-
Download Lecture Overview
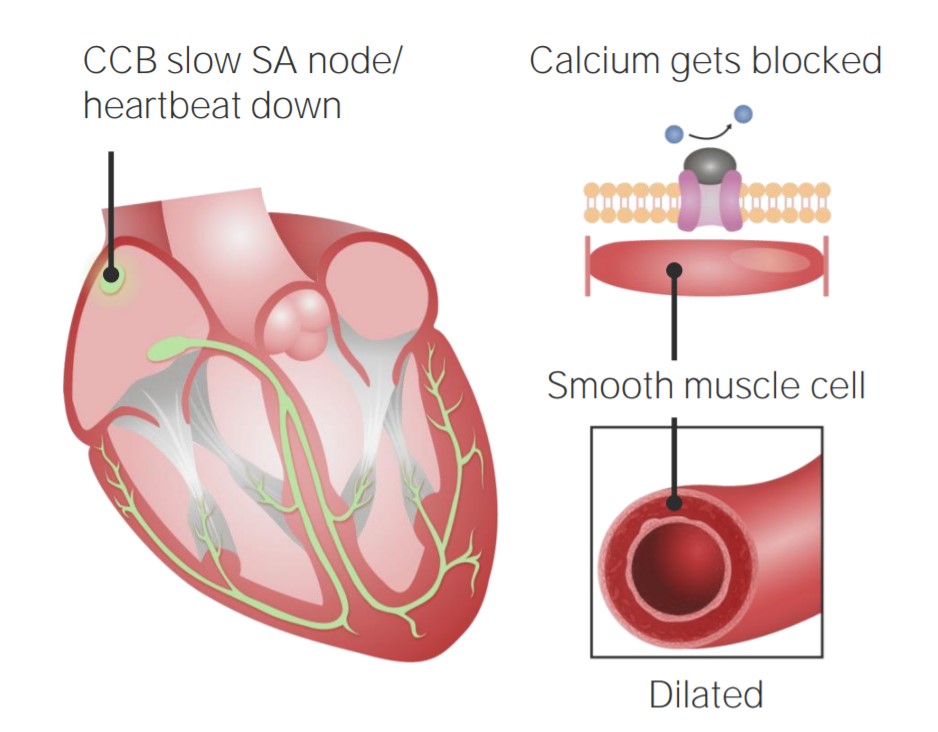
00:01 Welcome to Pharmacology by Lecturio. 00:04 We're going to cover today a strange disease called pulmonary hypertension. 00:08 It's not terribly common but I think it's important that you know how the drugs that treat it work. 00:15 Pulmonary hypertension just briefly is an elevated blood pressure within the pulmonary circulation, not the systemic circulation. 00:23 It is associated with shortness of breath, fainting episodes. 00:27 It can be associated with peripheral edema because you have an elevated right ventricular and diastolic pressure, and it can be associated with some tachycardia. We have several methods of treatment for pulmonary hypertension. 00:41 We have the calcium channel blockers, we have some vasoactive prostaglandins, we have some vasoactive endothelin antagonists, we have phospho-diesterase type 5 inhibitors, and we have guanylate cyclase activators. So, we have several different types of treatment available for this particular disease. 01:03 The first group that we'll talk about are the calcium channel blockers. 01:07 Remember these are exactly the same drugs that you see in hypertension so the names are the same, the method of activity is the same. 01:16 Unfortunately, we started to see an increased mortality in our pulmonary hypertension patients who were treated with CCBs because we weren't choosing our patients correctly. 01:27 Only 5% of pulmonary hypertension patients are truly vasoreactive. 01:34 Half of them do not respond long term in general to these agents, with respect to pulmonary hypertension, so, we have to be careful who we give them to. 01:45 Now, there's no mortality studies per se to support its use so we have to be aware as well, that the science doesn't support the use of CCBs in pulmonary hypertension. 01:57 That's not to say that some of the pulmonary hypertension specialist aren't using it, it's just to say that the science isn't as strong. 02:05 Now, we move onto the prostaglandins. 02:08 Essentially, we're talking about prostacyclin or prostaglandin I2. 02:12 These are the different types of agents that use prostaglandin I2 for the therapies. 02:19 They come under different types of therapies, and they come under different names, and they come under different injection mechanisms. 02:26 But bottom line, they're all prostacyclin.th The solution is clear with a pH of 10 which makes it kind of interesting from a pharmacology point of view. 02:35 Remember that if you're administering this agent and the solution is cloudy, you should be suspect that there's something wrong with the particular agent. 02:44 The effect is reversed after about 25 minutes. 02:47 There is no evidence of platelet dysfunction even though prostacyclin is associated with platelet activity control. 02:56 And finally, the side effects associated with this particular agent includes flushing; sometimes, you can get a headache because of vasodilation of cerebral arteries, and low blood pressure or hypotension because of vasodilation. 03:10 Now, if you look back to our lecture on inflammation, you saw me go through this very complicated graphic which has all this different complex molecules associated with the inflammation. 03:23 I just want to focus on one part of this and we're going to simplify this graph just to talk about prostaglandin I2. 03:31 So, let's take a look at the root product, sorry, the root of the production of prostaglandins. 03:39 We'll start out with the phospholipids. 03:42 Now, diacylglycerol or phospholipids are converted into arachidonic acid, either using phospholipase C or phospholipase A2. 03:51 The arachidonic acid is then converted into prostaglandin H2. So, what enzyme converts arachidonic acid into prostaglandin H2? Prostaglandin H2 synthase. 04:06 We also make prostaglandin D2. 04:09 And what enzyme makes prostaglandin D2? Prostaglandin D Synthase. 04:16 We have prostaglandin E2. 04:18 What enzyme makes prostaglandin E2? PGE synthase. 04:23 Similarly, we have prostaglandin F2, made by, you guessed it, prostaglandin F synthase. I'm not even gonna put it on the chart here, but we also have prostacyclin synthase that takes prostaglandin H2 and makes prostacyclin. Now prostacyclin and prostaglandin I2 are named the same thing, so to some people won't call it prostaglandin synthase, they'll call it PGI2 synthase, doesn't matter. 04:49 The point being is that you make prostacyclin or PGI2 from PGH2. Now, in the tissues, in the endothelium, you'll convert the prostacyclin into PGF 1 alpha, the 6-keto version of that. 05:05 So, this is the thing that's important for our disease state. 05:10 This is the area we're going to focus on. 05:12 The other part of it is just to give you an idea of where it fits into the armamentarium of treatment. 05:19 The next category of drugs are the endothelin receptor antagonists. 05:23 The first of these were called Bosentan that were introduced early in the 2000s. 05:28 We have other agents that have come on to the market since then. 05:31 These caused vasodilation directly at the level of the endothelin. 05:36 But unfortunately, because they are affecting the way the blood is flowing through various organs including the placenta, we don't like to give this to pregnant women. They are competitive antagonists of endothelin receptors, ET-A and ET-B. 05:52 They are substrates of two major enzyme groups. 05:56 First of all, the cytochrome system, types 3A4 and 2C9 so think cyclosporine in this case. 06:03 You will have an interaction with a lot of drugs because you are using the same pathway of breakdown as probably 60% of the drugs that are on the market. 06:12 So, be very aware of drug interactions when you're using this product. 06:16 The other thing that is a concern when you're using this medication is something called OATP. This is a type of anion-transporting system that is in the liver that is used to get rid of the drug from the body. 06:29 Remember that other drugs that go through this same system can have interactions with the endothelin receptor antagonists. 06:37 There's not a lot of them out there but just be aware that that can happen. 06:43 Another category of drugs used to treat pulmonary hypertension are phosphodiesterase type 5 inhibitors. 06:51 Now, you may be familiar with these drugs already because they're used in erectile dysfunction. The prototypical drug is Sildafenil which is also sold as Viagra for erectile dysfunction. 07:02 There are many other names that this is sold under for erectile dysfunction but it's also sold as a different name drug for pulmonary hypertension. 07:12 There are new analogs that have also come onto the market as well. 07:15 This has a relatively long half-life and as you are probably well-aware, it is an oral medication, which makes it convenient. 07:23 Side effects including those side effects that are associated with vasodilation so headache; sometimes you can get nausea; GI symptoms can occur as well like diarrhea; you can get backpain from this medication. 07:36 Other vasoactive type of side effects can include flushing, and myalgias, and you can also get a dyspepsia through an unknown mechanism. 07:46 How does this drug work? The mechanism of action is actually quite interesting. 07:51 Remember that PDE5 is associated with cyclic GMP degradation. If you inhibit cyclic GMP degradation, you have more cGMP available in the myocyte. 08:05 If you have more cGMP, you have vasodilation and relaxation of media within the blood vessel. 08:15 The next category of drugs used to treat pulmonary hypertension are the guanylate cyclase activators. 08:22 Now, the mechanism of action is kind of interesting. 08:25 You start off with a soluble GC. 08:27 It is the intracellular messenger for nitric oxide. 08:31 These drugs stimulate the soluble GC to do its job. 08:36 You end up having an increased biosynthesis of cyclic GMP, so you have more cyclic GMP in the system. 08:43 This causes an altered intracellular calcium flow into the cell, so it changes the actin-myosin contractility in the cell and you end up with vasodilation. 08:55 So, increasing amounts of cyclic GMP caused decreased intracellular calcium; decreasing intracellular calcium causes less actin-myocin interaction and therefore, you have more vasodilation. 09:10 We have two major drugs within this category. 09:13 One of them, Riociguat, acts independently of nitric oxide and it also increases the activity of the nitric oxide guanylate cyclase complex. So, to accentuate this Riociguat can work in concert with Nitric oxide to produce antiaggregation effects, antiproliferative effects, and the vasodilatory effects. 09:37 Okay, so, let's go through how this works in the real world. 09:42 You have two major enzyme systems. 09:45 The black part is the lumen of the blood vessels so the inside of the blood vessel; and surrounding the lumen is the endothelial cells or the endothelium. 09:55 Inside the endothelium, you'll have the nitric oxide system or synthase. 10:00 The smooth muscle cell is where the guanylate cyclase is. 10:05 So here you have, NOS or nitric oxide synthase, sometimes we call it eNOS because it's endothelial or endothelium nitric oxide synthase. 10:18 And here in the muscle you have the guanylate cyclase which we were talking about. Now, if you have a stimulus within the lumen, it can stimulate the nitric oxide system. 10:30 So, L-arginine which will be converted into nitric oxide will act on guanylate cyclase within the muscle layer of the blood vessel to convert GTP into cyclic GMP. Cyclic GMP causes that system to relax, so that's how you end up through the eNOS system to cause vasodilation. 11:00 So, when we look at the two drugs in this category, I mentioned the first one, I mentioned the second one first. 11:06 Now, let's talk about that first one. 11:08 Cinaciguat directly stimulates guanylate cyclase without going through the eNOS system. Riociguat has a dual mode of action. 11:15 It increases the activity of the nitric oxide guanylate cyclase complex and that increases cyclic GMP within the tunica media or the muscle layer of the blood vessel, and it also directly stimulates guanylate cyclase independent of nitric oxide.
About the Lecture
The lecture Pulmonary Hypertension Medication – Drugs in Hypertension by Pravin Shukle, MD is from the course Cardiovascular Pharmacology.
Included Quiz Questions
What is a common side effect of phosphodiesterase type 5 inhibitors, such as sildenafil (trade name, Revatio, when used for the treatment of pulmonary arterial hypertension, and Viagra, when used for erectile dysfunction)?
- Headache
- Increased blood pressure
- Drowsiness
- Rapid heart rate
- Muscle pain
What category of drugs used to treat pulmonary hypertension acts by increasing the amounts of cyclic GMP in the smooth muscle cell which causes decreased intracellular calcium, less actin-myosin interaction, and vasodilation?
- The guanylate cyclase activators
- Calcium channel blockers
- Prostaglandin I2 analogs
- Endothelin receptor antagonists
- Phosphodiesterase type 5 inhibitors
Customer reviews
1,0 of 5 stars
| 5 Stars |
|
0 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
2 |
2 customer reviews without text
2 user review without text