Playlist
Show Playlist
Hide Playlist
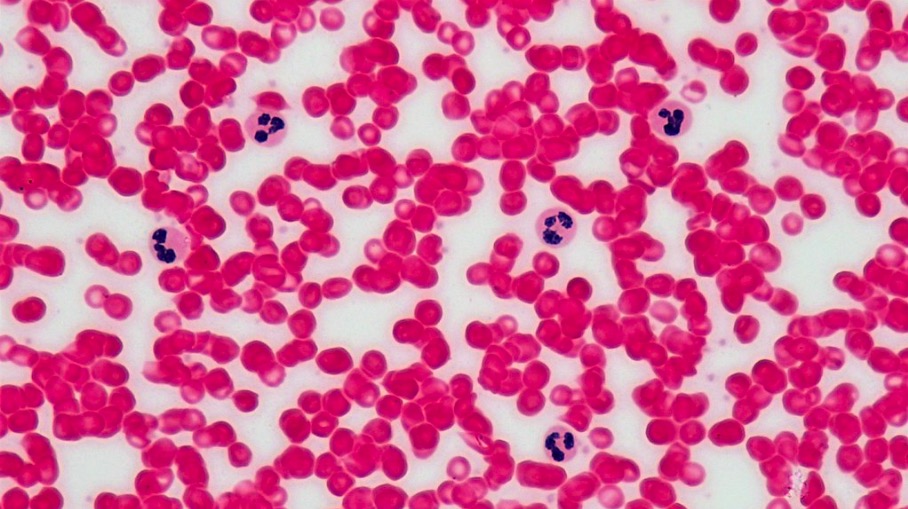
Neutropenia and Lymphopenia – White Blood Cell Pathology
-
Slides Quantitative Disorders.pdf
-
Download Lecture Overview
00:02 Neutropenia. 00:03 An absolute neutrophil count less than normal range. 00:07 Caused by: Myelodysplastic syndrome, megaloblastic anemia. 00:14 This is then referred to as being ineffective granulopoiesis. 00:18 "Dr. Raj, how in the world are you telling me a megaloblastic anemia causes neutropenia, or even for that matter, myelodysplastic syndrome? Because I find cells in my bone marrow. 00:28 In fact, I might actually find a lot of cells in my bone marrow, but yet you’re telling me neutropenia. 00:32 Look at the name, please. 00:34 Ineffective granulopoiesis. 00:36 You must call this neutropenia, because the type of cells that you’re going to produce in your bone marrow with MDS, which is more preleukemic in nature are megaloblastic in which your patient might be B12 or folate deficient. 00:48 You’re not going to form the proper functioning cells that you require. 00:52 Therefore, it may result in neutropenia or ineffective granulopoiesis. 00:56 Or bone marrow infiltration. 00:59 For example, leukemia, metastatic cancer, storage diseases, myelofibrosis. 01:03 Once again, here, it’s a space occupying lesion within the bone marrow rendering your patient neutropenic, neutropenic. 01:11 Splenic sequestration with splenomegaly. 01:14 There’s every possibility that the spleen itself may then sequester the neutrophil resulting in neutropenia. 01:20 But not just that, you could have neutropenia, anemia, or even thrombocytopenia when your splenomegaly look for those types of symptoms in your patient. 01:30 Drugs that cause neutropenia. 01:33 These are important. 01:34 Chemotherapeutic agents, alkylating, antimetabolite. 01:37 Remember, please, that chemotherapeutic drugs do what to your bone marrow? Shuts it down. 01:43 Bone marrow suppression. 01:45 In general, chemotherapeutic drugs like to target what kind of cells? What do you mean what kind of cells? Quiescent cells, stable cells, permanent cells, or labile cells, labile. 02:00 They love to go after cells that are constantly dividing, dividing, dividing. 02:04 That’s what chemotherapy is. 02:06 Chemotherapy is trying to attack those cells that are proliferating. 02:10 There’s every possibility that in addition to attacking the cancer, that might actually attack the bone marrow because in the bone marrow, oh my goodness, the amount of multiplication, normally, is a lot, and so therefore, it might shut it down bone marrow suppression. 02:26 Number two, tell me about the cells on the top of your head. 02:30 Hair loss, right? Because these are labile. 02:33 And what about the diarrhea? Good, the intestinal cells, which are also labile. 02:38 You knock out these three cells. 02:40 There are your symptoms for chemotherapy, uncomfortable, very uncomfortable. 02:46 Chlorpromazine, clozapine, atypical antipsychotic. 02:51 For this, every single month, you’re thinking about doing your proper granulocyte count so that your patient is not, is not susceptible to infection. 03:00 Sulfonamides and chloramphenicol, all may then cause neutropenia. 03:06 Lymphopenia is my topic, not neutropenia but lymphopenia. 03:10 Lymphopenia here will be, perhaps, due to HIV. 03:14 If it’s less than 200, automatically puts your patient on prophylaxis for pneumocystis carinii. 03:21 Autoimmune diseases may shut down your bone marrow lymphopenia. 03:25 Cytotoxic drugs, chemotherapy. 03:27 Glucocorticoid, long-term. 03:30 Let’s summarize real quick glucocorticoids. 03:33 Glucocorticoid given to your patient looks like Cushing looks like Cushing, buffalo hump, so on and so forth. 03:39 Glucocorticoid is then going to cause demargination, neutrophilic leukocytosis. 03:45 Glucocorticoids may then cause a decrease in lymphocytes, and perhaps even eosinophils due to apoptosis. 03:52 And glucocorticoids causes -- let’s say your patient comes in for a face lift, a plastic surgeon. 03:57 You’re giving glucocorticoid so that you can do -- well, slow down the wound healing on purpose. 04:04 Malnutrition. 04:05 Lymphopenia.
About the Lecture
The lecture Neutropenia and Lymphopenia – White Blood Cell Pathology by Carlo Raj, MD is from the course Quantitative White Blood Cell Disorders – White Blood Cell Pathology (WBC).
Included Quiz Questions
Which of the following does NOT cause neutropenia?
- Baclofen
- Leukemia
- Myelofibrosis
- Splenic sequestrations
- Megaloblastic anemia
Which of the following drugs can result in neutropenia?
- Clozapine
- Amiodarone
- Prednisone
- Carvedilol
- Amantadine
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |