Playlist
Show Playlist
Hide Playlist
Neuroepithelial Tumors
-
Slides 08 Tumors of the CNS Neuropathology II.pdf
-
Download Lecture Overview
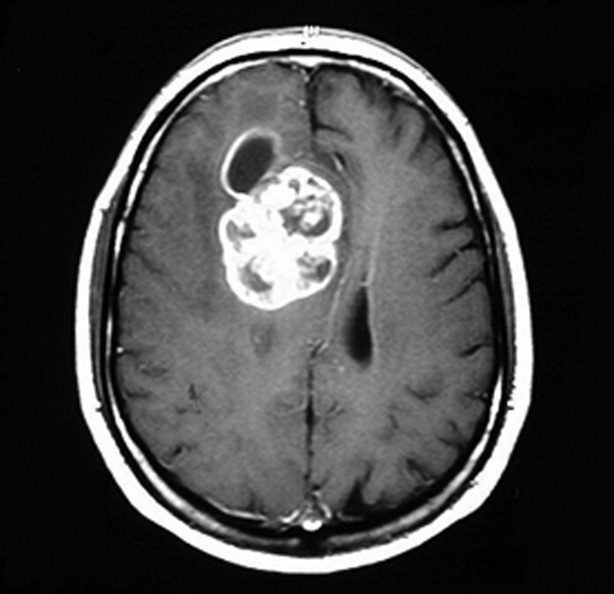
00:01 Now let’s get into Gliomas, Glioneuronal Tumors, and Neuronal Tumors. 00:07 These constitute the largest subset of neuroepithelial tumors and represent the majority of primary tumors of the central nervous system, abbreviated as CNS. 00:18 Their histological features are similar to normal glial cells containing astrocytes, oligodendrocytes and ependymal cells The diagnostic process begins with the light microscopy appearance, which is then integrated with the molecular and immunohistochemical findings. 00:37 These Tumors are categorized into 6 different families. 00:40 Adult-type diffuse gliomas are the most common primary brain tumors. 00:45 They manifest in three distinct forms, with one of them being Astrocytoma, IDH-mutant. 00:52 The isocitrate dehydrogenase mutation, short: IDH mutation, confers a better prognosis and can be grade 2, 3 or 4. 01:00 Grade 4 was perviously referred to as “IDH mutant glioblastoma” Oligodendroglioma, IDH-mutant is 1p 19q codeleted and can be grade 2 or 3. 01:10 The most common malignant primary brain tumor, Glioblastoma, IDH-wildtype is also known as “glioblastoma multiforme” and always categorized as grade 4. 01:21 The next family is the Pediatric type diffuse low-grade glioma, which generally results in a favorable prognosis due to its grade 1 classification. 01:31 In contrast, Pediatric-type diffuse high-grade glioma, graded as stage 4, is often associated with a poor prognosis. 01:41 Moving on to the family of Circumscribed astrocytic gliomas, it can be divided into three types. 01:48 Pilocytic astrocytoma is the most common glioma found in children and always classified as grade 1, with an overall favorable prognosis. 01:58 Pleomorphic xanthoastrocytoma can be grade 2 or 3, while a Subependymal giant cell astrocytoma, short SEGA is always grade 1 again. 02:09 Glioneuronal and neuronal tumors are glial cells showing neuronal differentiation and are mainly grade 1. 02:16 Lastly Ependymomas which are mainly grade 2. 02:21 Now let’s focus on the pathology of Astrocytoma, IDH-mutant. It often presents as WHO grade 2 but can also be grade 3 or 4. 02:31 Grade 4 is referred to as “IDH mutant glioblastoma”, with a mean age of only 35 years. 02:39 Initial management often involves observation if the symptoms are not serious, which is common for brain tumors. 02:46 The mean time to progression is approximately 4 to 5 years, and management after progression is usually surgical resection, radiation therapy, or a combination of both. 02:59 Mean survival after radiation and treatment ranges from 6 to 8 years. 03:03 Astrocytoma, IDH-mutant, grade 3, was previously called “IDH-mutant anaplastic astrocytoma”. 03:13 Patients with this conduction tend to be around 40 years, also relatively young. 03:19 Initial management includes surgery and radiation. Unfortunately, recurrence is almost certain, as Anaplastic astrocytoma is marked by a high mitotic rate. Progression to glioblastoma is frequent and can occur within two years. 03:35 Treatment following progression is symptomatic, involving surgical debulking, steroids for mass effect, and possibly chemotherapy. 03:44 Oligodendroglioma, IDH-mutant and 1p/19q codeleted, with grades 2 and 3, show varying ages of diagnosis. 03:56 It’s 43 years for a grade 2 tumor and 50 years for a grade 3 tumor. 04:01 They are slow-growing, infiltrative tumors often followed by seizures as their most common presenting symptom. 04:09 Treatment usually involves surgical resection and chemotherapy, with median overall survival ranging from 10 to 15 years for low grade tumors where 35 percent survive after 20 years. It’s 5 to 9 years for high grade tumors. 04:18 10 to 15 years for low grade tumors, where 35 percent survive after 20 years. It’s 5 to 9 years for high grade tumors. 04:26 Glioblastoma, IDH-wildtype, pay attention to this one, commonly still referred to as “Glioblastoma multiforme”. 04:36 It’s the most common malignant primary brain tumor and is always grade 4. 04:41 Mean age here would be 60 years with Necrosis or microvascular proliferation aiding in diagnosis. 04:48 Initial management includes maximal surgical resection and radiation, but even with these interventions, there's no guarantee. 04:55 Management after progression is symptomatic once again and chemotherapy can be required. However take a look at the survival. 05:04 Mean survival after initial treatment is only 1 to 2 years, which often makes the decision to pursue further treatment a complex matter that requires careful consideration and communication with the patient’s family. 05:18 Here’s a histologic picture of Glioblastoma multiforme. 05:22 Pay close attention to the surrounding border, which exhibits a pilocytic pattern of Glioblastoma multiforme. 05:30 This detailed understanding of histology is crucial, especially when dealing with adult astrocytomas. 05:37 Now let’s explore Circumscribed Astrocytic Tumors. Pilocytic astrocytoma is the most common glioma observed in children. 05:45 And the reason I'm being very technical here is because if there's a question at any point in time about what is the most common brain tumor overall, primary in a child? Then it will be medulloblastoma which we haven’t discussed yet. 06:00 Now let’s move on. It’s grade 1 classification is associated with a favorable prognosis. It typically occurs in children and young adults. 06:09 This cytic or cystic type of lesion is located in the cerebellum, which gives rise to specific clinical presentations. 06:18 The cerebellum in a child is still growing. It looks like a cystic like structure and whenever you think of a cystic it’s fluid filled. 06:28 Then what you're going to find in the middle of the cyst would be of what characteristic? The fluid appears to being lucent in this case and so therefore as it grows, it’s going to then impinge upon what? In front of the cerebellum. 06:42 So now you're talking about the fourth ventricle. If you start increasing the obstruction of the fourth ventricle, you are creating obstructive noncommunicating type of hydrocephalus. Symptoms usually include incoordination with walking, in other words maybe ataxia. A quick overview of some of the remaining astrocytomas. 07:03 Pleomorphic xanthoastrocytoma typically once again seen in children, could be found in younger adults as well. 07:11 It’s usually located in the temporal lobe and offers a progression free survival of 60 percent for grade 2 and 14 percent for grade 3. 07:21 Lastly SEGA, Subependymal giant cell astrocytoma. 07:26 It’s a periventricular tumor associated with tuberous sclerosis and is generally benign. Consistently graded as 1. 07:34 However, the risk of mortality and morbidity depends on the tumor’s size and location.
About the Lecture
The lecture Neuroepithelial Tumors by Carlo Raj, MD is from the course Tumors of the CNS. It contains the following chapters:
- Neuroepithelial Tumors: Fibrillary Astrocytoma
- Neuroepithelial Tumors: Glioblastoma Multiforme
- Neuroepithelial Tumors: Circumscribed Astrocytic Tumors
Included Quiz Questions
Which of the following is true about pilocytic astrocytomas?
- They occur in children, the lesions are cystic, and the location is cerebellar.
- They occur in adults, the lesions are cystic, and the location is cerebellar.
- They occur in children, the lesions are cystic, and the location is the cerebrum.
- They occur in children, the lesions are necrotic, and the location is cerebellar.
- They occur in children and adults, with cystic lesions.
Which of the following sites is most commonly affected in a patient with pleomorphic xanthoastrocytoma?
- Temporal lobe
- Parietal lobe
- Thalamus
- Pituitary gland
- Spinal cord
Which variant of astrocytoma is associated with tuberous sclerosis?
- Subependymal giant cell astrocytoma
- Pilocytic astrocytoma
- Glioblastoma multiforme
- Pleomorphic xanthoastrocytoma
- Anaplastic astrocytoma
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
clear and concise in explanation; content well-organized and presented in a way that is easy to absorb