Muscles of the pelvic floor
By Leocadia N. on 07. November 2022 for Arrhythmias: Basic Principles with Carlo Raj
Excellent concise and precise. Oh! I love how Dr. Raj emphasize on important these. Cracks me up and keeps me engaged. Thanks
Excellent teacher Dr carlo
By Arjit S. on 15. August 2022 for Arrhythmias: Basic Principles with Carlo Raj
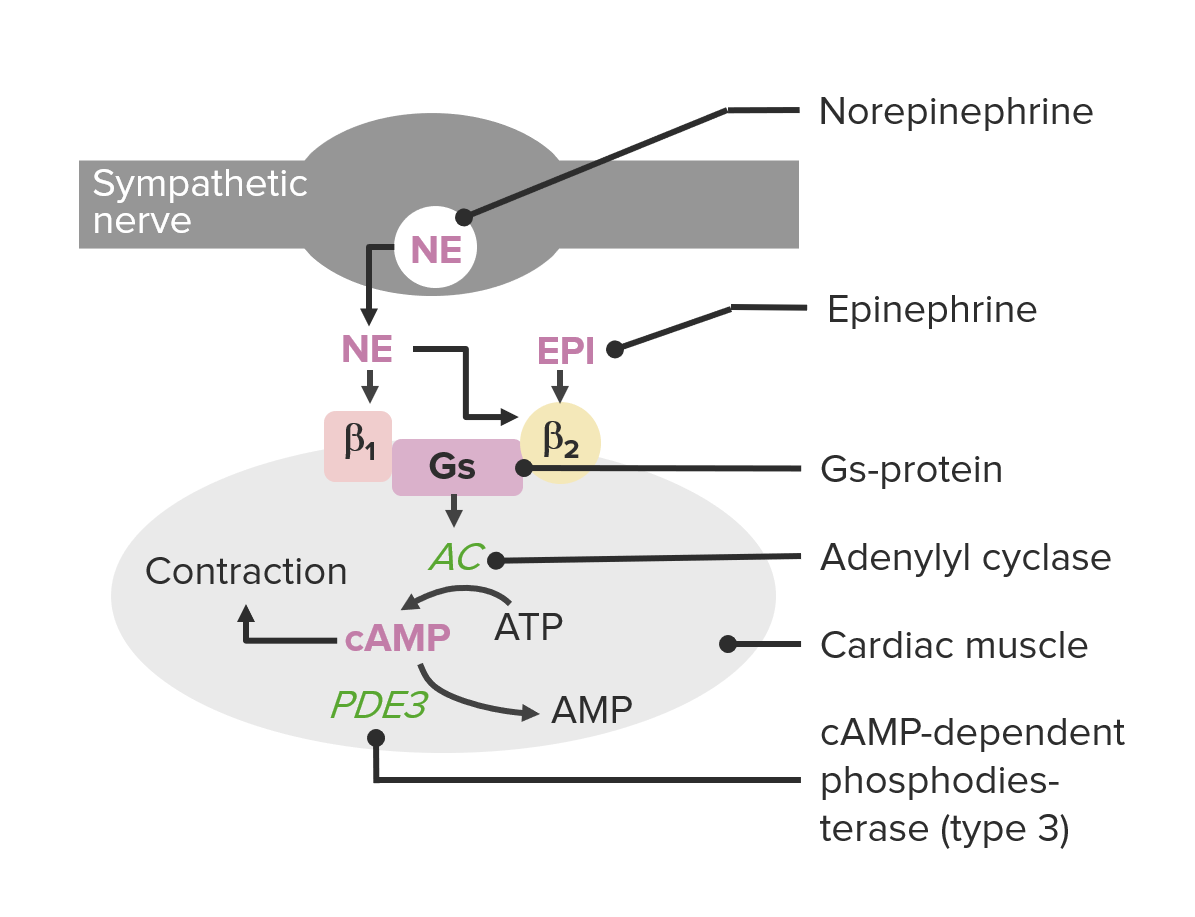
Dr Carlo gives maximum emphasis on conceptual understanding of the topic rather than just reading slides
Very good and to the point course regarding atrial fibrillation.
By Lan d. on 22. December 2021 for Arrhythmias: Basic Principles with Carlo Raj
Dr. Raj is very good. He is a bit fast and I sometime have a difficult time to clearly hear him. Your price range is a bit too high for retired people like me who would like to learn practical things like the EKG, endocrine system etc… just enough to better understand our doctors if and when we have a health condition.
Great lecture!
By Nara A. on 20. October 2021 for Arrhythmias: Basic Principles with Carlo Raj
Great course, well explained, love how he connects the physiology with the lectures so you can see how they are related.
Best of the lecturio!
By Yiğit Kağan A. on 26. August 2021 for Arrhythmias: Basic Principles with Carlo Raj
Dr. Raj is my fav lecturer on here without a doubt. He's teaching excellently. I really am angry towards morons who have suboptimal Iq for med school and make comments about how Dr. Raj is bad lol. I wish all lecturers were like Dr. Raj, to be honest. I really don't like to see lecturers who try to simplify as much as possible. They're teaching like you're an idiot. It's not really unfortunate that people who have suboptimal Iqs don't love Dr. Raj which is fine BUT please don't try to remove Dr. Raj lectures and replace the old lectures.
very enlightening
By Rob. W. E. on 24. August 2021 for Cardiac Arrhythmia: Dysrhythmias and CSD
very well outline and simplified presentation. Good wits combined with serious discussion
Thanks!
By S C. on 17. August 2021 for Bradycardia: Sinus Bradycardia and Heart Blocks
very good intro to heart blocks. I think next few lectues would also help if details are provided.
Good high yield material!
By JOSE ANTONIO P. on 08. March 2021 for Arrhythmias: Basic Principles with Carlo Raj
Quick and concise great delivery of a difficult topic, obviously get the basics first before this lecture!
Great pharm tips for understanding
By Keila O. on 08. March 2021 for Tachycardia: Wolff-parkinson White Syndrome: Diagnosis and Treatment
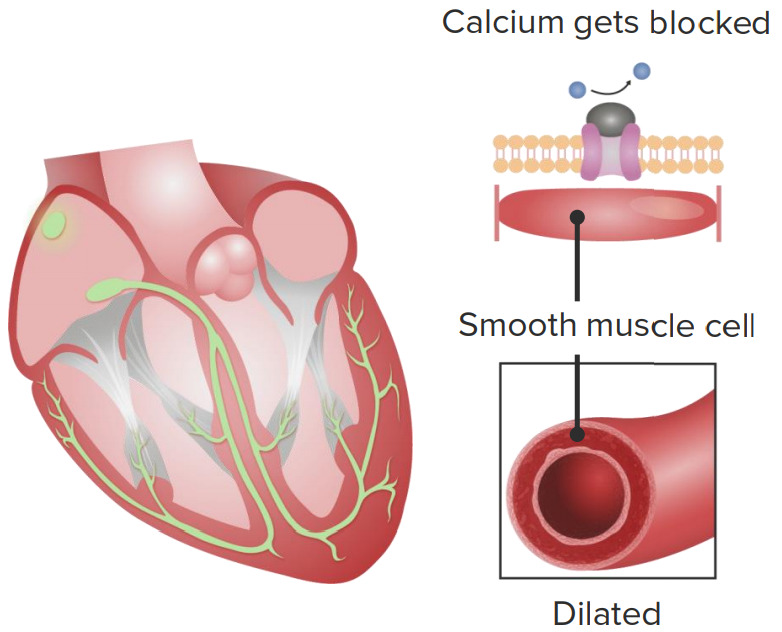
I love how he explains why CCBs and digoxin are contraindicated in WPW and also review of how digoxin isn't useful for MAT
Great lecture!
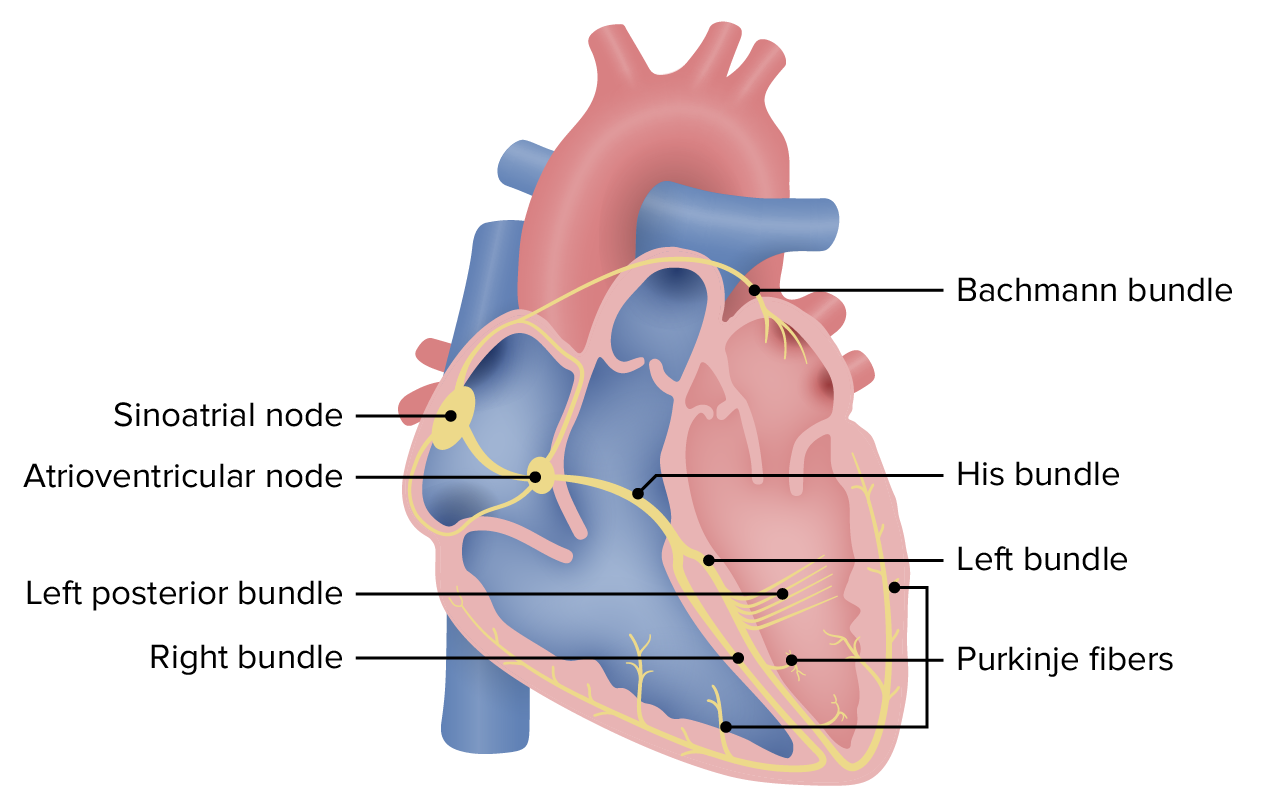
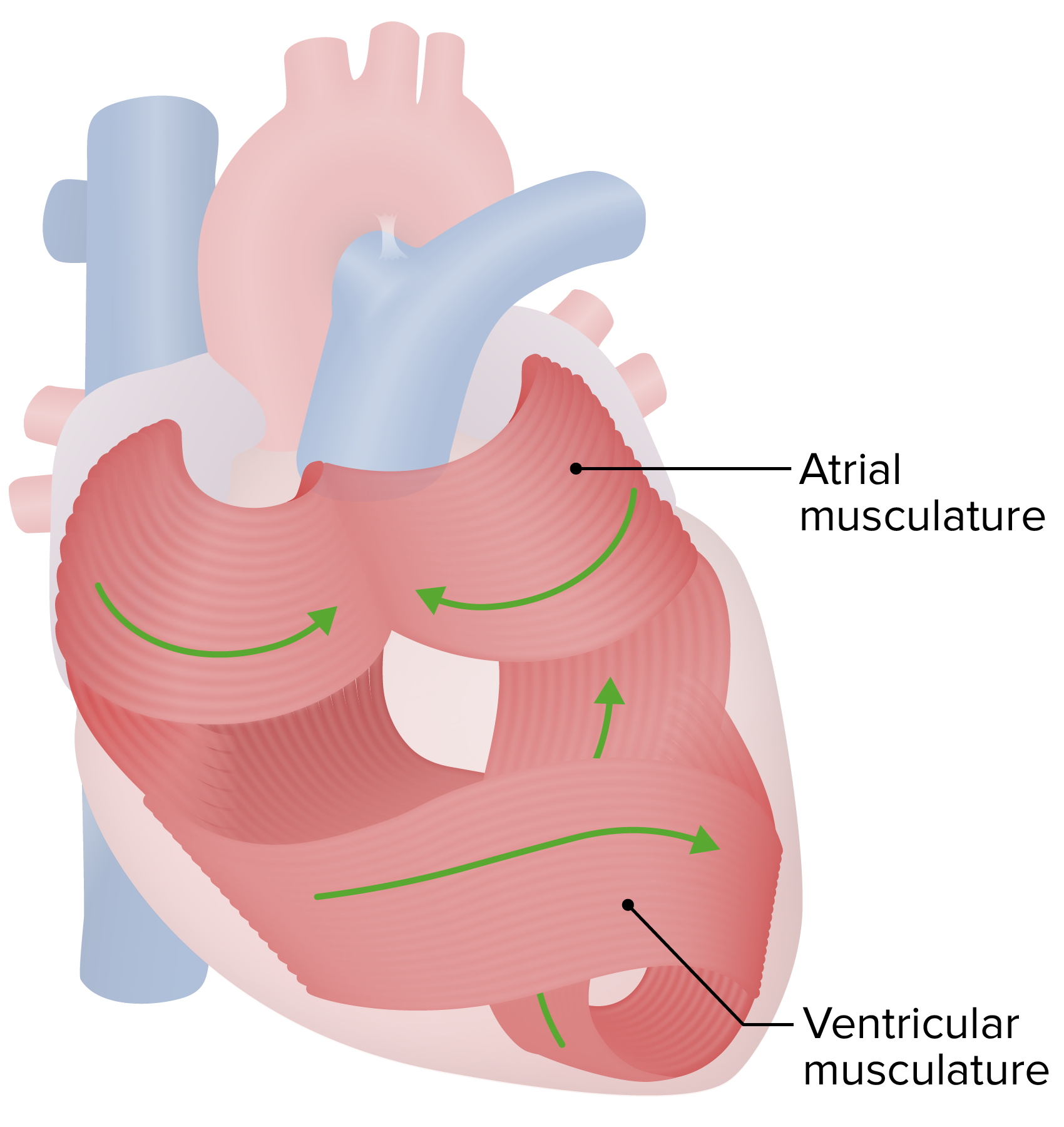
By Keila O. on 08. March 2021 for Cardiac Arrhythmia: The Electric System of the Heart
Great integration of concepts in EKG, heart sounds, etc. Dr. Raj does not disappoint!
Understanding the entire picture!
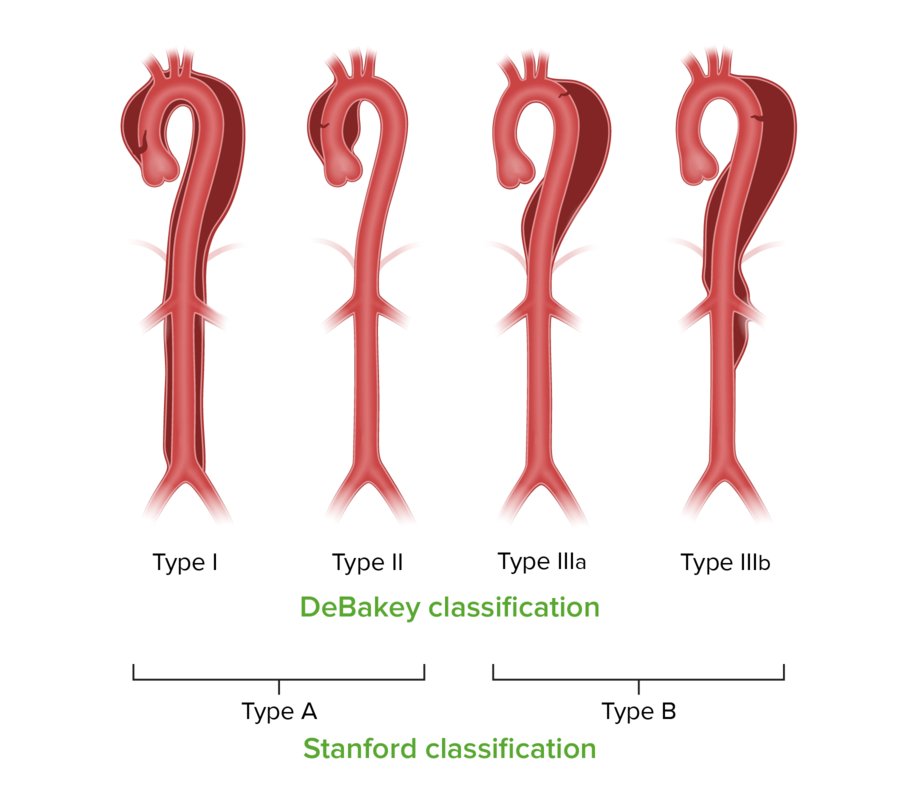
By Carol M. on 27. February 2021 for Aortic Dissection: Signs, Symptoms, Diagnosis and Treatment
If you want your education to elevate to another level, to be ready for rotations, and to be the best medical professional you want to be....listen to DR. Raj!
5/5
By Athanasios S. on 20. January 2021 for Cardiac Arrhythmia: Review
Dr. Raj lecture is filled with “dramatic expressions” that made understanding/memorizing information easier. Dr. Raj appears to be passionate about his work, making his lectures enjoyable.
Integration of basic knowledge and understanding
By Barbara E J. on 09. January 2021 for Arrhythmias: Basic Principles with Carlo Raj
Whereas I was at first put off a bit by Dr. Raj's style of teaching, I became more and more appreciative of his pedagogic method, soliciting and emphasizing the integration of basic physiology, pharmacology and anatomy in understanding and treating (the pathology underlying) clinical syndromes (of the multiple organ systems). Indeed, the process becomes very stimulating and ultimately satisfying as one becomes able to retrieve and integrate all the basic knowledge in solving clinical diagnosis and treatment.
Buena correlación entre fisiología, clínica y farmacología
By José V. on 09. December 2020 for Tachycardia: Atrial Fibrillation: Treatment
Muy completa la explicación y clara, además de correlacionar muy bien la fisiología con la clínica y semiología. Muy buenos tips semiológicos.
Excellent!
By dipen p. on 04. November 2020 for Arrhythmias: Basic Principles with Carlo Raj
An excellent way of explaining the abnormal rhythms associated with different pathologies!
Awesome!!
By Caridad G. on 01. October 2020 for Arrhythmias: Basic Principles with Carlo Raj
Great teacher! I highly recommend Lecturio. It has allowed me to master Arrhythmias and all of Cardiology.
Amazing lecture!
By Maria M. on 30. June 2020 for Second Degree Heart Block
Such a great and objective lecture! Amazing teacher and materials, thank you
thanks for the course
By Talal H. on 08. June 2020 for Arrhythmias: Basic Principles with Carlo Raj
excellent course very easy and simple + covering the most high yield topics.
Dr Raj - Brilliance in summarized format
By Muhammad K. on 05. May 2020 for Arrhythmias: Basic Principles with Carlo Raj
Dr Raj is brilliant.
His lectures are fun to watch, concise, high yield and his expressions are captivating to the student.
His manner of teaching makes you think critically and apply your knowledge
Great lecture, but points for improvement :)
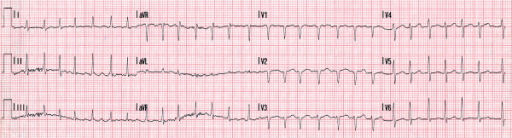
By Kevin C. on 14. April 2020 for Third Degree Heart Block
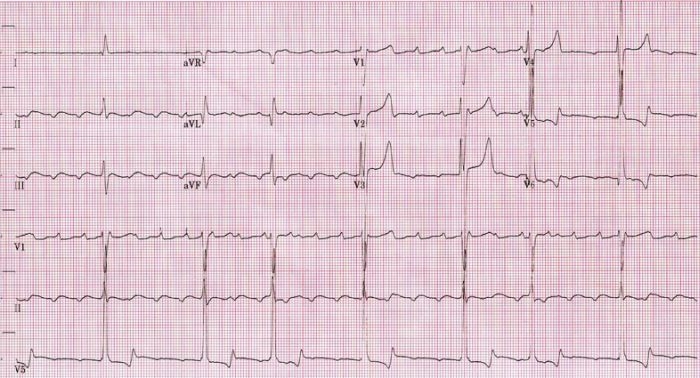
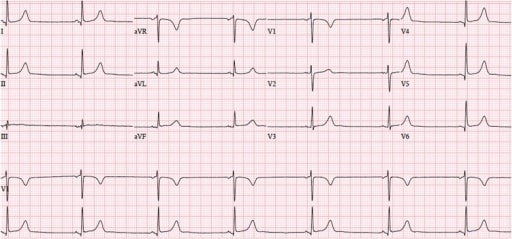
Great lecture as always, but could be improved with more depth into the morphology of how the QRS complexes can be either narrow or wide depending on the site of the block.
Could also be improved through:
- A list of specific symptoms a patient with the condition would experience
- ECG interpretation in the quiz section
I like that this lectore repeats the main information so I know what is neccessary to know
By Ivan K. on 11. September 2019 for Tachycardia: Atrial Fibrillation: Diagnosis
I like that this lectore repeats the main information so I know what is neccessary to know
Excellent lecture
By Osa G. on 07. July 2019 for Arrhythmias: Basic Principles with Carlo Raj
I’m so glad there are lectures like him. Challenges you, keeps you engaged and wanting to learn more.
Great
By Juliette K. on 03. July 2019 for Arrhythmias: Basic Principles with Carlo Raj
Dr Raj explains it really well and he has great humor
He is a king in teaching>>
By ARCHANA R. on 23. March 2019 for Arrhythmias: Basic Principles with Carlo Raj
One of the best teachers i have come across. He makes the lecture so interesting and the voice modulation prevents us from getting distracted......Awesome teacher.
very clear and effective lessons
By samantha r. on 02. February 2019 for Arrhythmias: Basic Principles with Carlo Raj
one of the best lecturer that i have seen. thank you very much,the way he is doing easy to remember all the facts.
clarification regardong ebsteins anomaly
By Joseph S. on 05. December 2018 for Tachycardia: Wolff-parkinson White Syndrome: Definition and Pathogenesis
you seem to skip over Ebsteins anomaly and it kinda seems like you're saying it's a side effect of lithium. it isn't. it's a CONGENITAL anomaly that presents in neonates whose mother took lithium during pregnancy.
Welcome to
By Mikholae H. on 30. November 2018 for Arrhythmias: Basic Principles with Carlo Raj
Dr. Raj has a teaching style that makes the content just stick. I sometimes hear him in my head when doing a question, and actually said to a patient when explaining "welcome to Sjögren's Syndrome" once.
muchas gracias
By Fernanda A. on 11. September 2018 for Tachycardia: Atrial Fibrillation: Pathogenesis
Explica exactamente lo que es, me ha ayudado mucho para dar un exposicion del tema
The easiest way to learn fast and efficiently your arrhythmias with Dr Raj!
By Dr Jerry G. on 02. February 2018 for Arrhythmias: Basic Principles with Carlo Raj
I learn so fast and easy all the most know arrhythmias with Dr Raj.
He is fun, knows how to teach, blue print materials, great pics and graphs. I never learned that well my dysrrhythmias before my lectures with Dr Raj.
Bravo Dr Raj! My grades are improving big time. I wish I had you as a teacher before.
Than you so much Lecturio and Dr Raj!
Ridiculously good!
By Sandra F. on 20. January 2018 for Arrhythmias: Basic Principles with Carlo Raj
Dr. Raj is the best! He is funny and he makes arrythmias ridiculously simple. I recommend his lectures for everyone!
Outstanding
By Mikholae H. on 28. October 2017 for Second Degree Heart Block
Very much appreciate his teaching style, but does stray some at times.
concise information
By Geovannia G. on 27. October 2017 for Arrhythmias: Basic Principles with Carlo Raj
I like this video becaus of concise explanation on etiology, patho and Treatment
Thank you Lecturio! ????
By Antoinette D. on 06. October 2017 for Arrhythmias: Basic Principles with Carlo Raj
Thank you for your commitment to medical education. I am sure that many medical professionals and students are benifiting in an enormous way from Lecturio!
I liked it
By Andre K. on 29. September 2017 for Arrhythmias: Basic Principles with Carlo Raj
It is summed up and easy to understand and becoase of this it is a great start to the arritmias study.
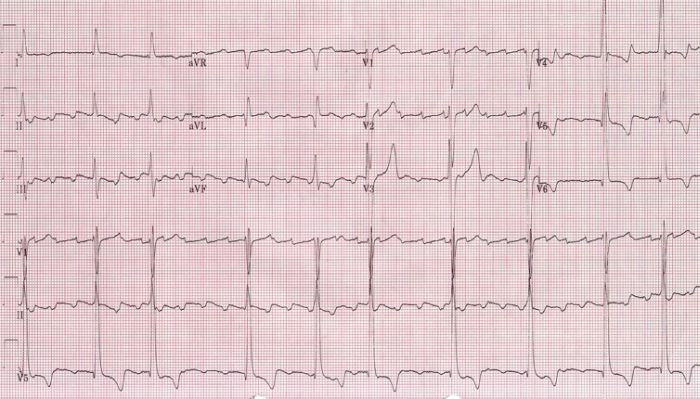
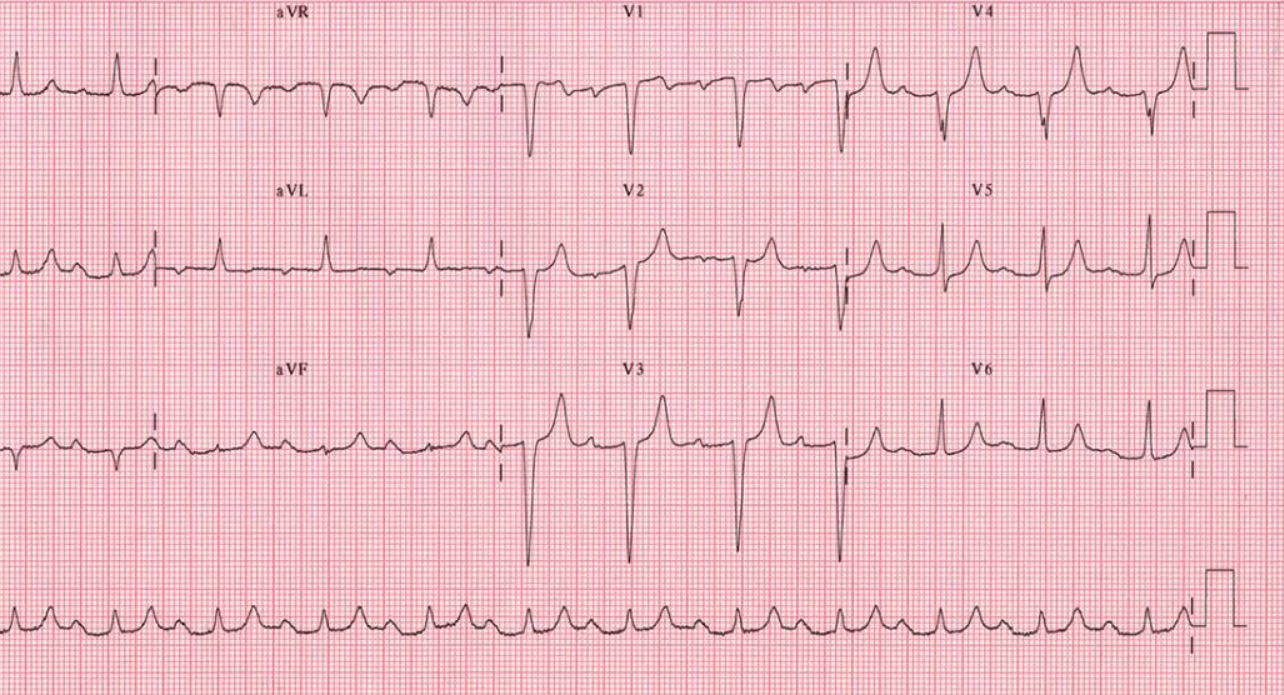
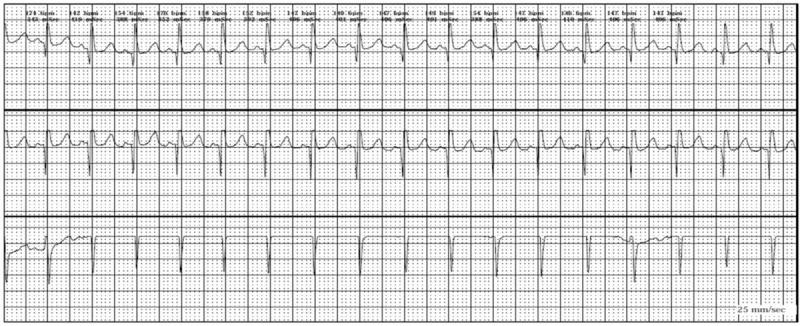
EKG
By DIANA C. on 26. December 2016 for Arrhythmias: Basic Principles with Carlo Raj
Lecture is Great I would like to see more EKG 12 lead on step to read them
Diana