Awesome
By Omoniyi Henry A. on 30. July 2023 for Glomerulonephritis
Awesome
It explained it down to the nitty gritty aspects
Much appreciated
Excellent explanation by Dr. Raj
By Manuel T. on 24. April 2023 for Minimal Change Disease
Too good, is what I was looking for the topic
Many thanks to a dr. Carlo Raj about course Glomerulonephritis.
By Gulbanu S. on 10. February 2023 for Glomerulonephritis
Hello lecturers Team
Brilliant lecturers from Dr C. Raj.
Especially differential diagnostics in terms of pathology.And diff diagnostics are outstanding.
Glomerulonephritis
By Desiree E. on 13. May 2022 for Glomerulonephritis
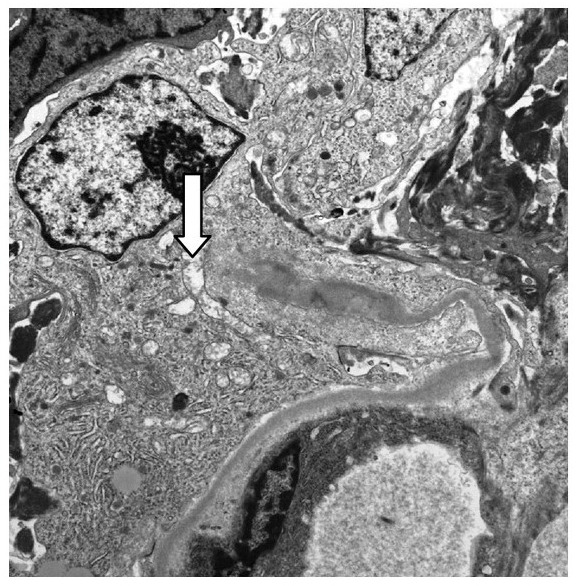
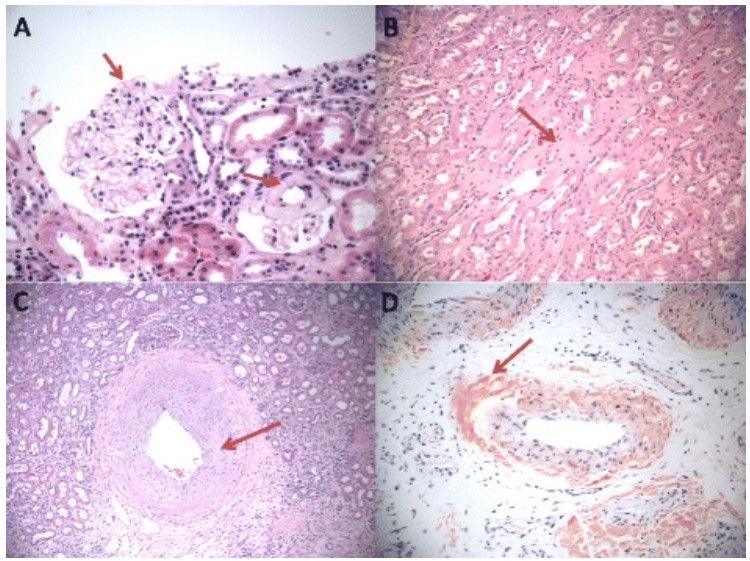
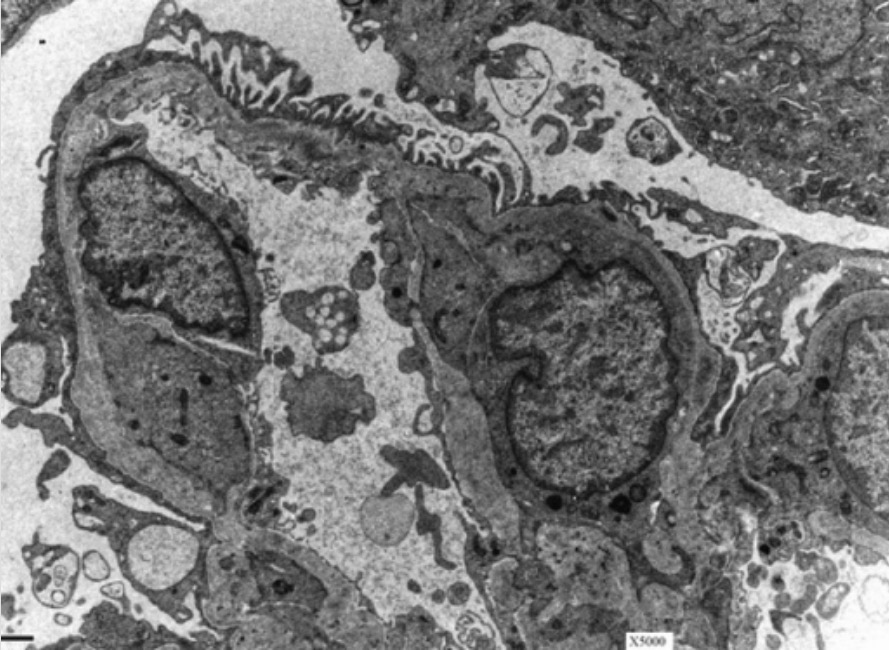
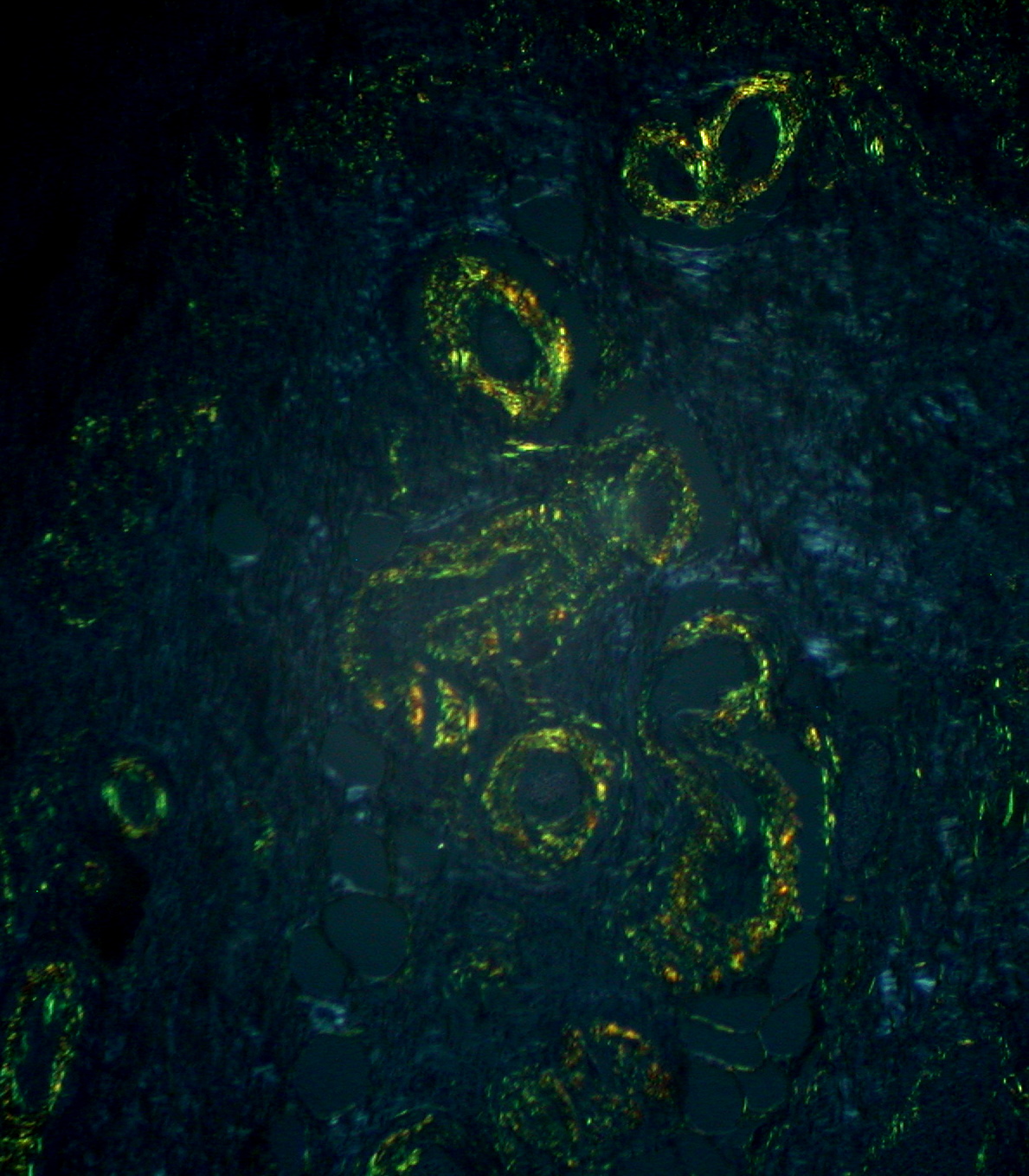
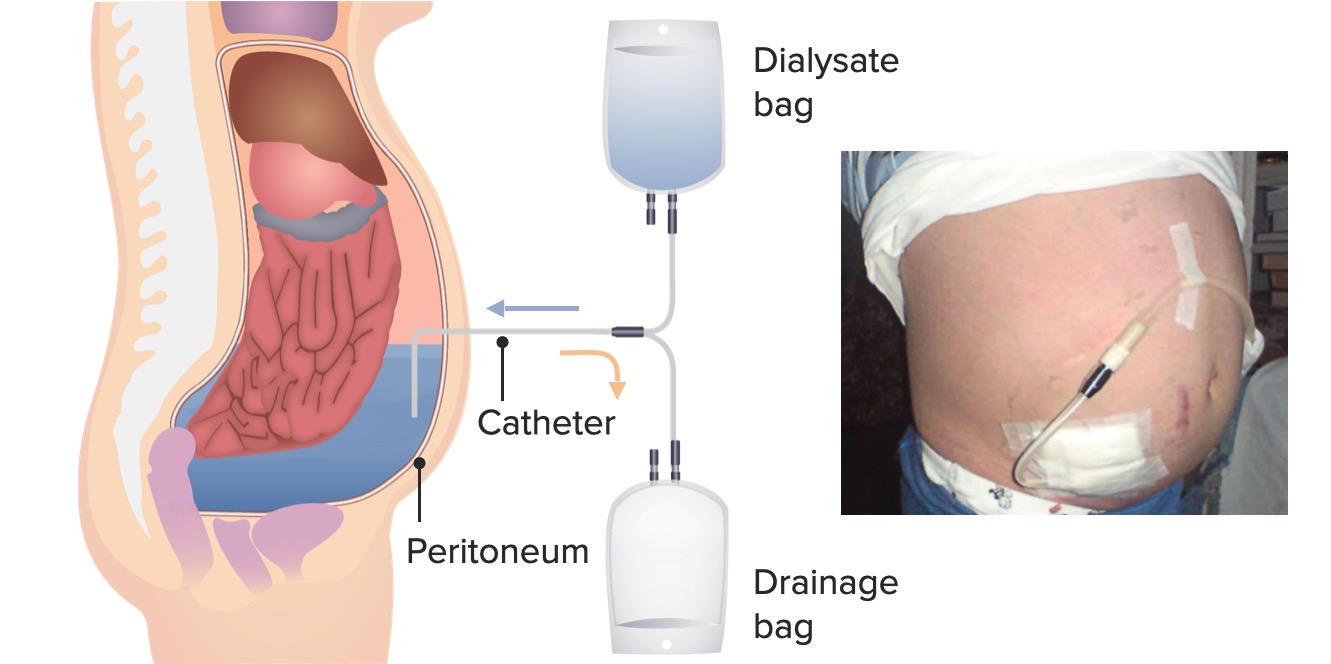
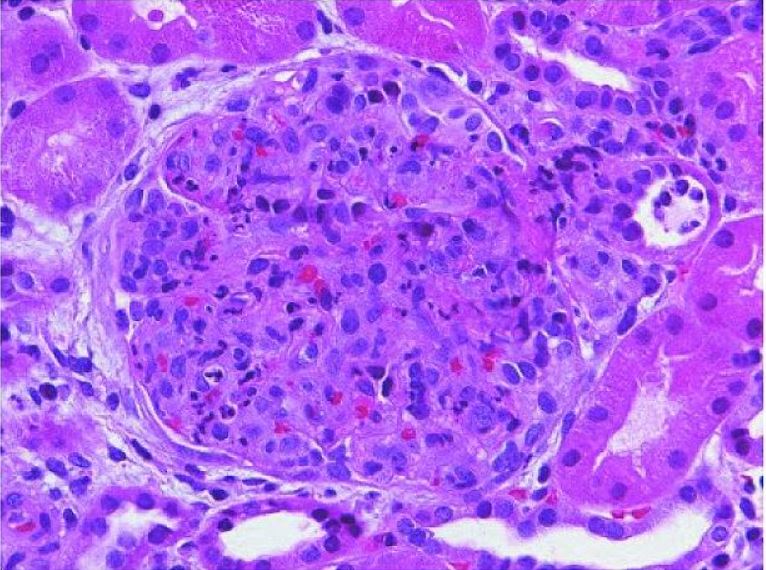
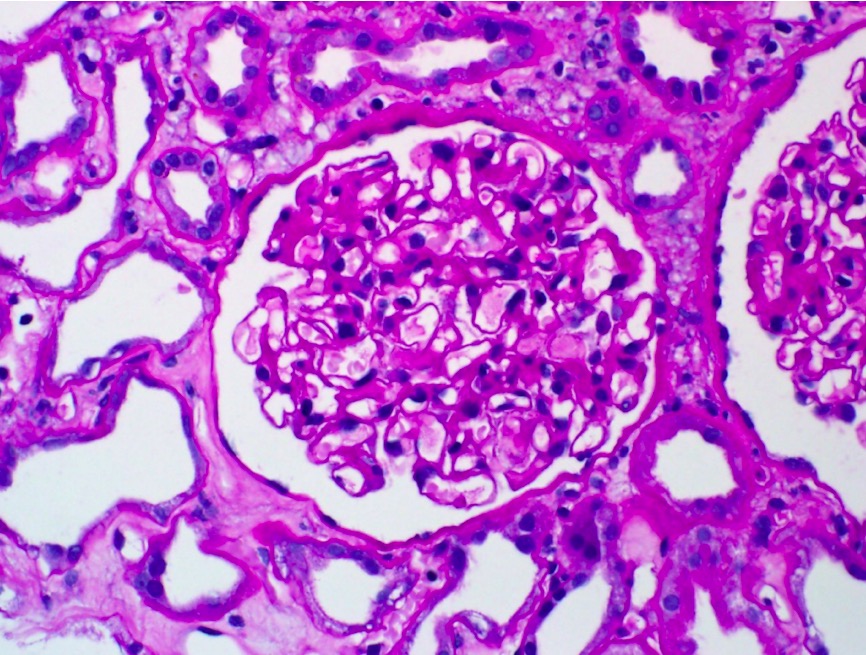
The lectures are pretty good but many of the ddx are dependent on the histo, EM, IM, etc findings. PLEASE provide a pointer for future lectures. Simply describing what we should be seeing is not as helpful - it's difficult to follow along.
Great lecturer, great lecture
By Deniz Y. on 25. January 2022 for Post-Streptococcal Glomerulonephritis
Dr Carlo Raj is excellent teacher that manages to keep me both attentive and interested in the topic. He seems to have a good understanding of key topics and what is important to medical students.
Wonderful lecture by doctor raj
By Chandra S. on 28. October 2021 for Glomerulonephritis
Well explained .Full of concepts and differentials.and gud humour
Amazing Dr. Raj
By Ignacio R. on 23. June 2021 for Glomerulonephritis
Great summary and extraordinary explanation of each one of the diseases
Informative
By Neuer N. on 12. May 2021 for Types of Glomerular Diseases
Dr C Roy has a very pragmatic approach that makes more sense when recalling
Amazing!
By FRANCICO FLAVIO C. on 29. April 2021 for Diabetic Glomerulopathy esp. Kimmelstiel-Wilson Disease
Congratulations!
Complete review !!! Excelent, high level questions. Best review I have seen about the topic!
Great
By Inaamul Hassan J. on 21. March 2021 for Glomerular Disorders
Enthusiastic, to the point, interesting lessons which are enjoyable and educational
Highly recommended
By majdee M. on 16. December 2020 for Glomerulonephritis
Couldn’t be done better thank you dr raj ,very helpful
Very well explained
By Luis V. on 24. July 2020 for Glomerulonephritis
I loved the lecture, I learned things I didn’t know. Like it very much.
Not clear
By Carlos W. on 29. June 2020 for Glomerulonephritis
The content is great, it's just hard to understand. Dr Raj knows a lot, but it's hard to understand everything. So it's like a Ferrari without wheels, you have the power, but it struggles getting you somewhere. It's not the ideal scenario with something like this, like pathology, and because of the amount of content in the program. Like I said, other than that, great.
Good
By Ravi G. on 06. May 2020 for Glomerulonephritis
Was good lecture .........but can you expand more on diagnosis and treatment
Very good explanations, more images and a pointer needed.
By Francisco Javier S. on 01. May 2020 for Glomerulonephritis
The explanations are very good and concise. Nonetheless, specially in these topics, we need to see more images, there are a lot of glomerular damage patterns even for the same disease (e.g. FSGN) and I do not think there were enough images to learn them. Also, a pointer is needed, Dr. Raj described numerous glomerular lesions and sometimes it was difficult to follow his descriptions as he didn’t have a pointer to help him locate those lesions.
Even with these problems I really liked how Dr. Raj really emphasized the diseases patterns and reminded them almost in every video (E.g. SubEPIthelial in PSGN).
Dr. Raj is hilarious!! Will keep you hooked.
By Fleming M. on 11. April 2020 for Glomerulonephritis
Dr. Raj Explains topic with finesse and maintains the balance with his quirky dialogues.
Great
By 顥 懷. on 08. March 2020 for Glomerulonephritis
Organized and informative. Made me remember the key points easily. A pointer is needed to illustrate the graphics.
helpful
By jinxiu p. on 20. February 2020 for Glomerulonephritis
very clear, and easy to remember all the points, and it is very helpful to understand
Excellemt
By Ali O. on 04. February 2020 for Glomerulonephritis
Great presentation, complete and educational. Questions are very helpful. Thank you
I understood the glomuruler disease like ever befor really thanks alot
By rania a. on 20. December 2019 for Glomerulonephritis
excillent lecture ,Teacher and presentation ,Just recommend to use pointer when Explain on dighram .
excelent teacher
By Ricardo G. on 17. November 2019 for Rapidly Progressive Glomerulonephritis (rpgn) & Subtypes
The best teacher , his sense of humor make the lectures more fun
Glomerulonephritis
By Nguyễn Minh H. on 20. July 2019 for Glomerulonephritis
He explained many problem in glomerulonephritis very clearly. I 'll appreciate that.
Great video
By Admitere B. on 29. June 2019 for Rapidly Progressive Crescentic Glomerulonephritis
Doctor, you are great! I've been struggling with nephrology for some time, and after trying many sources and attending multiple classes, I can finally say I found something that really makes everything very clear.
I'm having some really beautiful days studying now. Thank you!
Excelent explanation
By Ismael Francisco V. on 13. June 2019 for Glomerulonephritis
There was a profound description of physiopathology, with emphasis on the clinical elements that helped lead to diagnosis.
There was a lack of precision regarding diagnostic cut-off values, treatment and follow-up.
Like It Very Much!
By Anwr A. on 09. April 2019 for Glomerulonephritis
The lecture is awesome, It really helped me understanding Glomerulonephritis. The lecturer is excellent, slides are excellent, repeating was crucial for this topic. I would recommend this to all medical students, who are struggling to understand Glomerulonephritis. Very Helpful.
thank you so mush it was helpful
By gumaa a. on 07. April 2019 for Glomerulonephritis
thank you so mush it was helpful thank you so mush it was helpful
FABULOUS!
By Anne c. on 23. February 2019 for Glomerulonephritis
Dr. Raj is great! His presentations are interesting, to the point and you DO learn, even when somewhat tired. I enjoy and look forward to seeing these lectures.
Great!!!!!!!!
By James A. on 08. November 2018 for Glomerulonephritis
Thank you Dr Raj!!!! finally understand this complicated topic. Dr Raj is the best.
Glomerular diseases
By adrianmola2014@gmail B. on 17. April 2018 for Post-Streptococcal Glomerulonephritis
It was great because I achieved to understand in detail a very complex topics. Thanks
One of the best!
By Mariana I. on 31. May 2017 for Glomerulonephritis
Great presentation, great explanations.
At the end, finally, everything fits into their place! wonderful.
GN review
By Tereza K. on 03. January 2017 for Glomerulonephritis
thank you for the lecture!
I really like how you repeat multiple times the important key facts. Also the presentation with comparisons and simple key facts instead of too much material is really nice.
The best thing, you actually made me think through the whole lecture compared to just passively listen.