Playlist
Show Playlist
Hide Playlist
Medications for Non-Parkinsonian Movement Disorders
-
Slides Medications for Non-Parkinsonian Movement Disorders.pdf
-
Download Lecture Overview
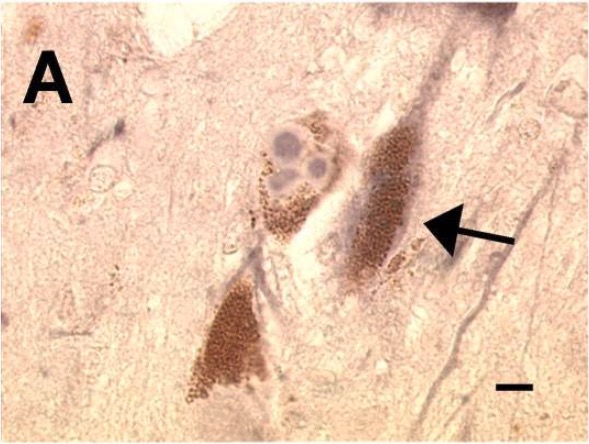
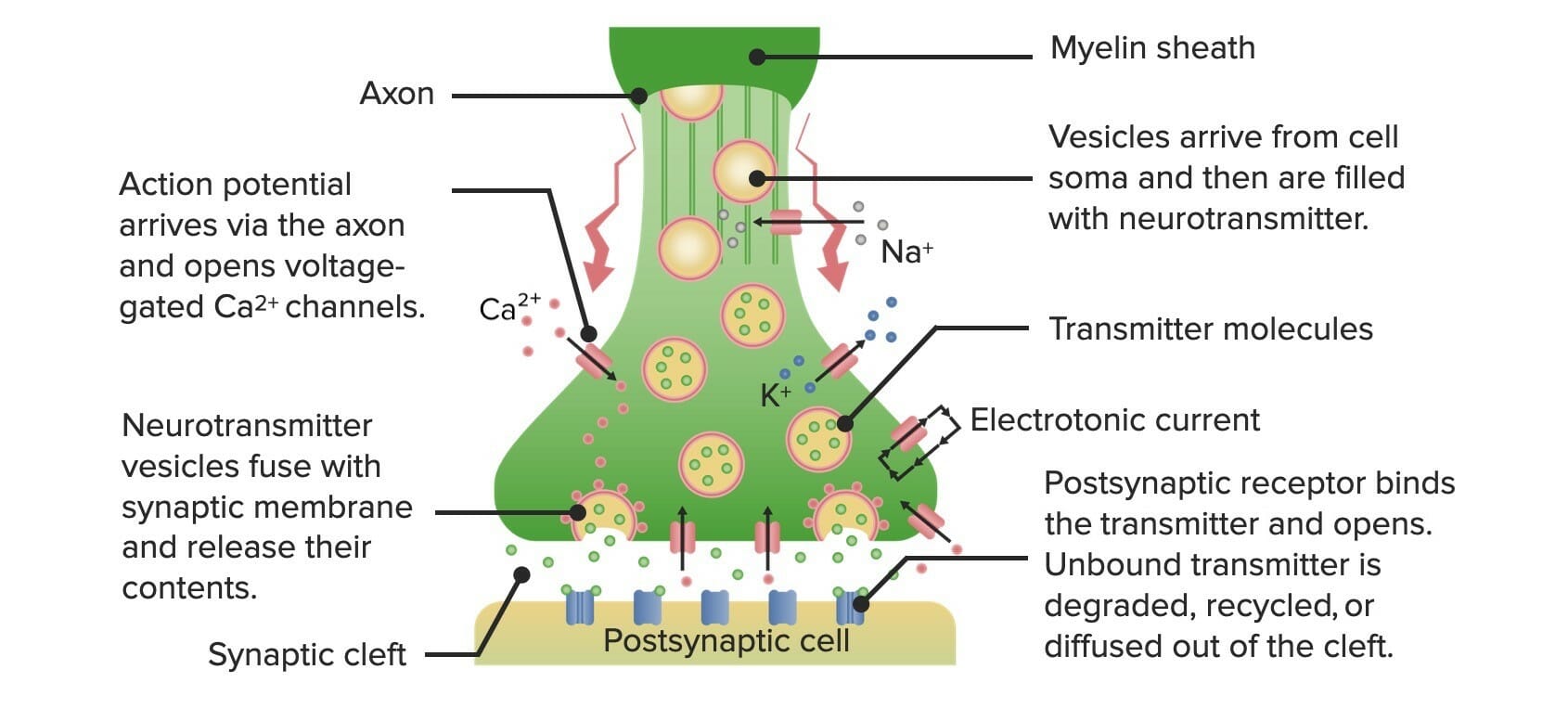
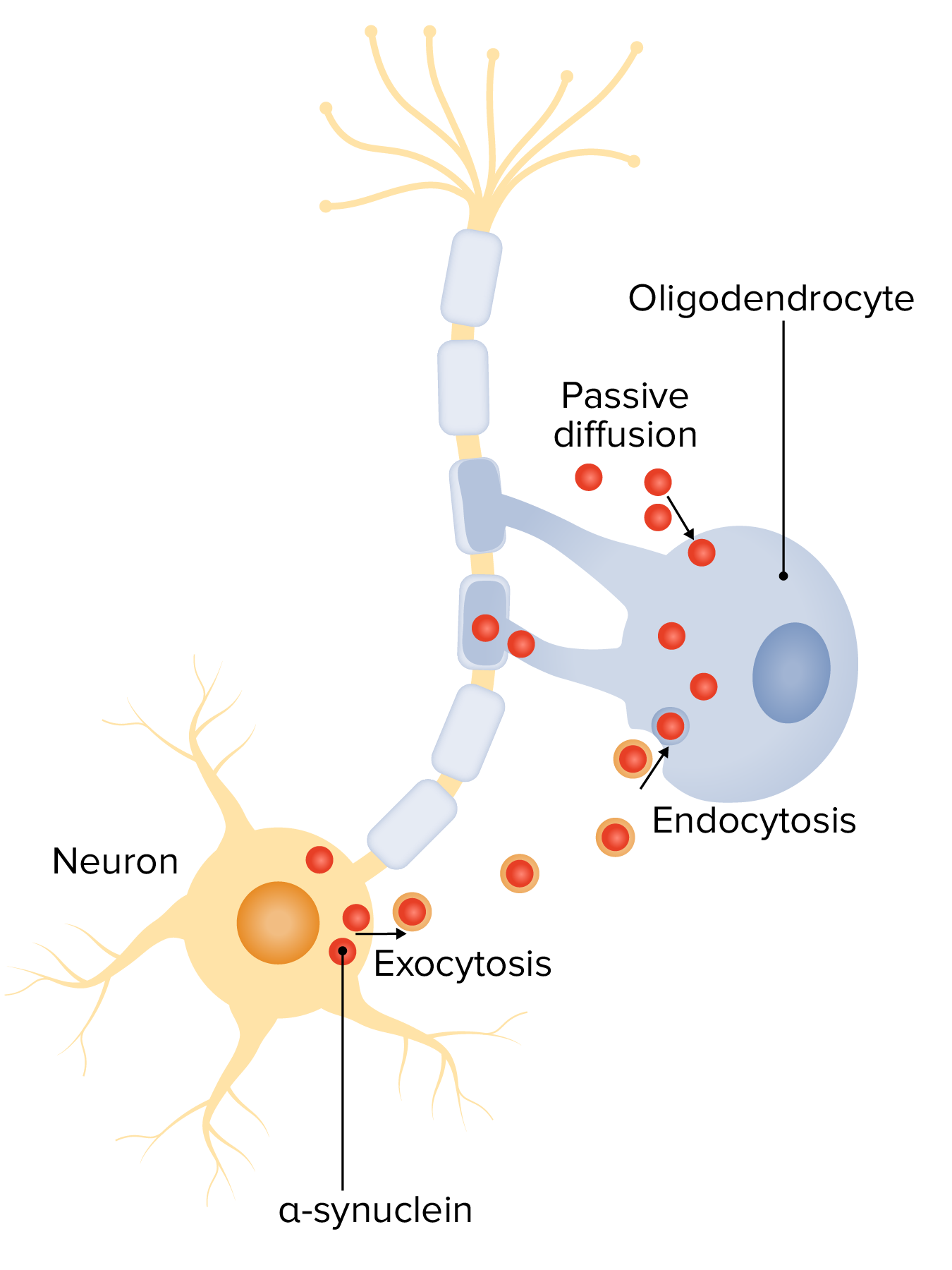
00:01 We're going to talk now about drugs used to treat other movement disorders or what we call non-parkinsonian movement disorders. 00:09 We're going to start off first with tremor. 00:11 Now you're going to cover tremor much in much more detail in your neurology lectures I'm only going to talk about the medications. 00:19 Propranolol is a beta blocker. 00:22 Other beta blockers can be used as well. 00:24 Propranolol is a very effective agent in postural tremor. 00:28 It seems to respond well to beta blockade, we're not exactly sure why that happens. 00:34 Gabapentine, primidone and topiramate are also anti-epileptic drugs that may also work in postural tremor. 00:43 Huntington's disease is a complex, choreiform type of movement. 00:47 It's inherited. It's passed on. 00:50 It affects the GABA function. 00:53 So by giving medications to affect GABA function, we can reduce Huntington's disease. 00:59 These medications include those which deplete the storage of dopamine or block dopamine transmission. 01:05 Vesicular monoamine transporter type 2 (VMAT) inhibitors, such as tetrabenazine and deutetrabenazine, act by depleting dopamine storage in presynaptic vesicles in CNS. 01:16 They should not be used if the patient also has depression, agitation, or psychosis. 01:22 Antipsychotics work by blocking dopamine transmission. 01:26 The second-generation antipsychotics, such as risperidone, are preferred over the first-generation ones, such as haloperidol. 01:34 Benzodiazepines can be provided as needed. 01:37 Because these drugs interfere with dopamine, the patient must be regularly monitored for signs for parkinsonism. 01:44 In many Huntington disease patients, chorea peaks at approximately 10 years after the first signs of disease, followed by declining choreiform activity while bradykinesia and rigidity become more prominent, so different therapies would then be necessary. Tourette syndrome also responds to dopamine depletion or transmission blocking, which means using VAMT2 inhibitors or antipsychotics Alpha adrenergic agonists, such as guanfacine and clonidine can be useful. They are also used to treat attention-deficit hyperactivity disorder known as ADHD. The blood pressure must be monitored because they cause hypotension. 02:26 Botulinum toxin injection is possible for focal motor or phonic tics or if there are violent neck extension tics. 02:33 In complex cases or comorbid epilepsy, other drugs have been used, such as antiseizure medications, like topiramate and carbamazepine, as well as benzodiazepines and cannabinoids. Wilson's disease. 02:46 Now, Wilson's disease is generally thought that it was liver disease. 02:51 The classical finding in Wilson's disease is a Kayser-Fleischer ring that's seen in the eye on eye exams. 03:00 So you can see a little bit of a brown haze on the edges of the iris. 03:05 This is a disorder of copper metabolism. 03:07 Why am I talking about it here? Because it does result in neurological damage. 03:13 Myasthenia can occur, and mild movement disorders that are very nonspecific can occur in Wilson's disease. 03:21 This is why, just as a clinical pearl, always do a good eye exam in your patients and take a close look at their iris, because you may actually pick up Wilson's disease. 03:30 I've done it a couple of times in my own patients. 03:33 The treatment is penicillamine. 03:35 Now, penicillamine chelates copper out of the blood. 03:39 So if you can give them penicillamine early enough, you can actually treat the movement disorder associated with Wilson's disease. 03:47 Restless leg syndrome is a common movement disorder characterized by an uncomfortable urge to move the legs during sleep or other periods of inactivity, and which is relieved by moving the legs. 03:59 The cause is unknown. In approximately 50% of the cases there is a family history of RLS. 04:07 Comorbid conditions which are commonly associated include low iron stores, uremia, neuropathy, spinal cord disease, and pregnancy. 04:18 The pathophysiology may involve reduced central iron stores or alterations in dopaminergic pathways and other neurotransmitters. 04:27 For treatment, iron supplementation is given if the serum ferritin is less than 75 micrograms per liter, and/or if transferrin saturation is less than 20 percent. 04:36 Alpha-2-delta calcium channel ligands like gabapentin enacarbil and pregabalin are considered first-line therapies; they inhibit calcium mediated neurotransmitter release, but their actual role in RLS is unknown. 04:51 Dopamine agonists, such as pramipexole, ropinirole, are effective in the treatment of RLS. 04:56 Carbamazepine (Tegretol) may also be useful in the treatment. Opioids are reserved for treatment of severe RLS but must be used cautiously because of side effects and potential for abuse. 05:10 Next we're going to talk about dystonia. 05:12 Dystonia refers to sustained or intermittent muscle contractions, usually focal. 05:16 Examples include: retrocollis, torticollis, opisthotonus, hyperextension of the arms or legs, blepharospasm, and jaw dystonia. 05:25 Examples of opisthotonos and retrocollis are shown in this slide. 05:29 There are many types and multiple causes of dystonia; most are idiopathic, but they may be acquired, as in certain CNS pathologies or by certain drugs. 05:39 Inherited causes are rare. 05:41 The most prevalent form of dystonia is idiopathic cervical dystonia. 05:45 The pathogenesis is uncertain, but two mechanisms are suggested. 05:49 Abnormal dopaminergic activity in the basal ganglia is likely, since dopamine receptor antagonists such as antipsychotic drugs and metoclopramide can cause dystonia. 05:59 Abnormal cholinergic activity is also a strong possibility, since anticholinergic therapy can be effective. 06:07 For the treatment of acute drug-induced dystonia in adults: stop or change the drug and give anticholinergics, such as trihexyphenidyl or benztropine. 06:17 For other dystonias in adults, if it is drug-induced when it also called “tardive dystonia,” although some authors consider it a type of tardive dyskinesia: Stop or change the drug if possible. 06:28 For the remaining types of dystonias, a trial of levodopa should be tried, to exclude a rare dopa-responsive dystonia. 06:36 Botulinum toxin injection is the preferred therapy. 06:40 If that is not possible, or if there is not a good response, the benzodiazepines and anticholinergics are used. 06:47 Other medications which may be employed include baclofen, which activates the GABA-beta receptor, thereby inhibiting the release of excitatory neurotransmitters. 06:57 A vesicular monoamine transporter type 2 inhibitor such as tetrabenazine may be given if there is generalized isolated dystonia. 07:06 Finally, deep brain stimulation if the dystonia is refractory to other treatments. Next up we're going to move on to tardive dyskinesia. 07:15 Tardive dyskinesia, or TD, is a drug-induced hyperkinetic movement disorder, usually occurring in orofacial muscles, associated with the use of dopamine-receptor-blocking agents, such as antipsychotics—especially the first-generation ones, or anti-emetics, such as metoclopramide or prochlorperazine. 07:36 The most important risk factors are older age and length of drug use; TD developed in a about half of the patients who took a first-generation antipsychotic for 10 years. 07:47 Other risk factors are people with fetal alcohol syndrome, other brain disorders, and diabetics. Women are more affected than men. 07:55 The pathophysiology of TD is not understood, but possible mechanisms include chronic blockade or damage of D2 receptors, which causes increased levels of glutamate in the striatum, with consequent excitotoxic destruction of GABA- and peptide-containing neurons. Another possible mechanism involves the production of free radicals which are generated by increased neuronal dopamine turnover. 08:20 For the prevention of tardive dyskinesia, use the lowest effective dose of antipsychotic drugs. 08:26 Screen for TD every 6 months sing the Abnormal Involuntary Movement Scale (AIMS)* because TD may become irreversible. 08:34 For metoclopramide or prochlorperazine, avoid continuous use for more than 12 weeks. 08:40 The treatment of TD involves discontinuing the drug if possible, using a lower dose, or switching to an anti-psychotic with lesser risk for TD (e.g., risperidone, clozapine, quetiapine). 08:54 For mild TD, benzodiazepines are advised, while for moderate to severe TD, the vesicular monoamine transporter type 2 inhibitors are indicated, such as valbenazine, deutetrabenazine, and tetrabenazine): these drugs deplete dopamine storage in presynaptic vesicles in CNS. 09:14 Deep brain stimulation is recommended for refractory TD. 09:18 So there you have it. These are the non-parkinsonian movement disorders. 09:25 I'm sure you'll do very well on your exams.
About the Lecture
The lecture Medications for Non-Parkinsonian Movement Disorders by Pravin Shukle, MD is from the course CNS - Pharmacology. It contains the following chapters:
- Postural Tremor
- Huntington's Disease
- Tourette's Syndrome
- Wilsons's Disease
- Drug Induced Dyskinesia
Included Quiz Questions
A female presents to your clinic with occasional sporadic movements of her upper and lower extremities. She reports these symptoms started recently and have been progressively getting worse. She vaguely remembers her father had a similar condition, but he died when she was very young. Which of the following conditions is most likely?
- Huntington disease
- Wilson disease
- Postural tremor
- Tourette Syndrome
- Drug-induced dyskinesia
A 17-year-old female presents to your clinic because of abnormal uncontrolled limb movements over the past few months. She has no history of a serious illness. On physical examination, her liver is slightly enlarged. Blood results reveal elevated liver enzymes. Which finding is associated with the most likely diagnosis in this patient?
- Kayser-Fleischer rings
- Pill-rolling tremor
- Abnormal movements or speech patterns
- Cotton wool spots and hemorrhages in the retina
- Arcus senilis
Pharmacotherapy for Tourette syndrome includes dopamine antagonism. Which drug is the most appropriate in this regard?
- Tetrabenazine
- Bromocriptine
- Carbidopa
- Pergolide
- Omeprazole
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |