Playlist
Show Playlist
Hide Playlist
Male Hypogonadism
-
Slides Reproductive Hormonal Pathophysiology.pdf
-
Download Lecture Overview
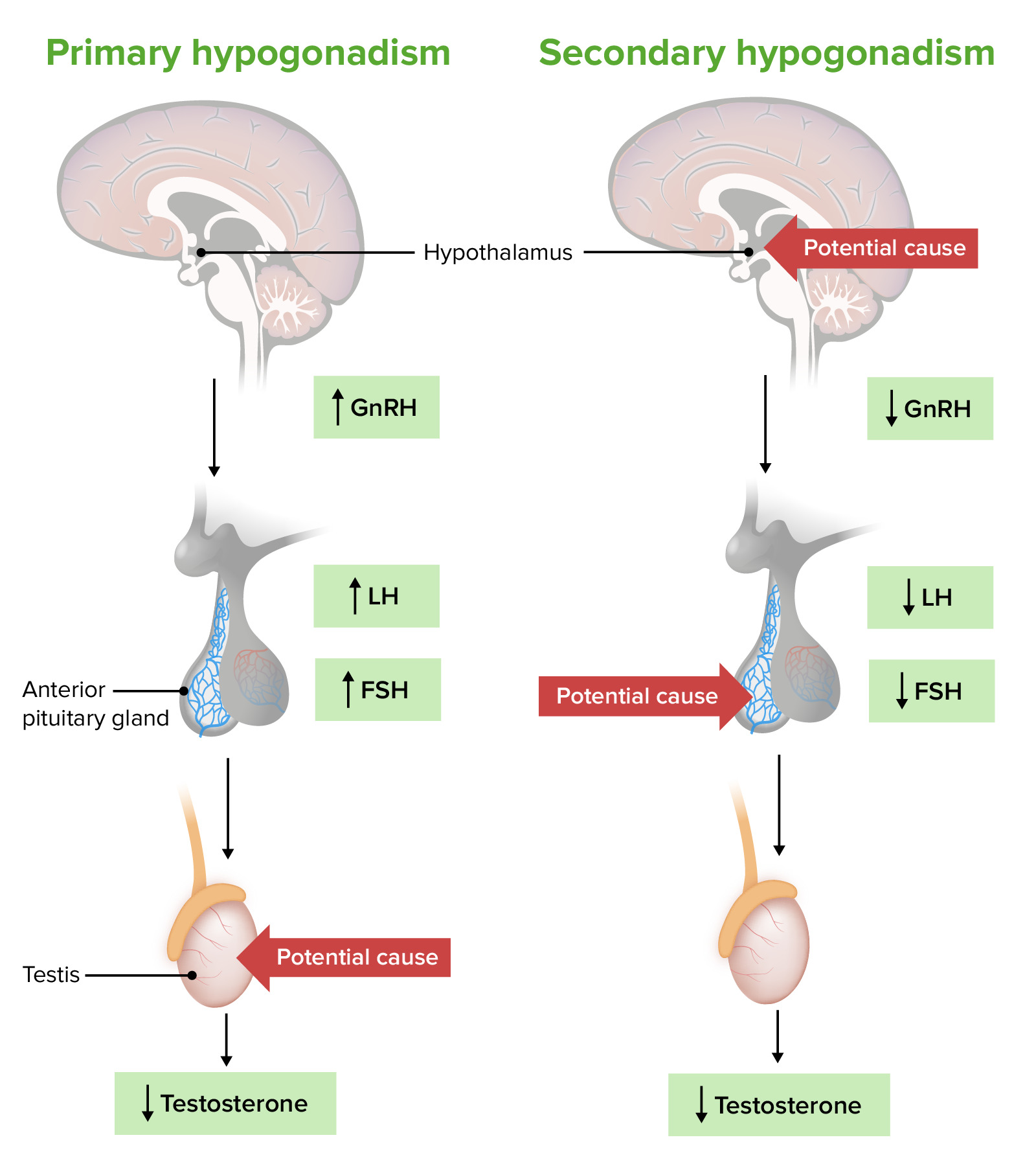
00:01 Our topic is male hypogonadism. What happened here? Well walk through maybe primary hypogonadism. Normal range is about 713, 1300 ng/dL. Take a look at your age, 18 to 29. 00:15 You want there to quite a bit of testosterone. What then happens after the age of 70? Do you understand this? The fact that if there is any chance of a male becoming infertile, It might be average age of approximately 70. So, during that whole time, not every patient obviously because as I said low-T syndrome is a real thing in clinical practice in the US. 00:41 Classification: what if it’s a primary testicular dysfunction? What would you call this? We talked about this in previous table. Take your time here. We call this primary hypogonadism. 00:53 How would you call this pathophysiologically? You would call this hypogonadism. The testis are not functioning properly. You would have increase in LH and FSH, so primary hypogonadism, A.K.A., hypergonadotropic hypogonadism. Clear? Secondary, central. You put together pituitary, hypothalamus. I've told you to do that a number of times, secondary or perhaps tertiary, secondary anterior pituitary, tertiary hypothalamus. If that’s knocked out, what do you call this clinically or pathophysiologically? Hypogonadotropic hypogonadism. 01:37 Causes of male hypogonadism. Primary: trauma, autoimmune destruction. Do not forget about mumps and microbe, orchitis. Inflammation of the testis, inflammation of the parotid, orchitis, parotitis. Medications: cyclosporine, chemotherapy. Congenital disorders: Well talk about Klinefelter big time and something called bilateral anorchia. In other words, it's the fact that, my goodness gracious, congenital, the testis won’t even properly develop. 02:09 Primary, why do we call it hypogonadotropic. Are we clear? Do I sound like a broken record yet? Good, I should. You want me to because you want to get bored with what I’m saying because Dr. Raj, I know this. Stop talking. Hypogonadotropic, hypogonadism. Secondary causes: Where’s my problem? Head, automatically go to head. Put together hypothalamus and and pituitary. Technically, it’s secondary and tertiary, anterior pituitary, hypothalamus respectively. Chronic illness. Medications such as opioids, glucocorticoids, leuprolide. 02:45 What? Yes. When? I’ll walk you through this one more time. You’re giving gonadotropin releasing hormone continuously. At first, you’re going to have, you put your foot on the accelerator pedal to the metal, increase LH and FSH. But that wouldn’t give you hypogonadism. The objective clinically is to actually decrease LH and FSH release. 03:08 When would you use this? I told you about prostate cancer. What are the receptors? What’s the name of the drug that will then inhibit the receptors on the prostate? Flutamide. 03:18 Other causes of secondary: This one I have to remind you, have to. Chances are you're either a little shady right now with this information. I'm here to instill confidence. 03:29 Prolactinoma. Let’s say that your patient has MEN-1. Pan, para, pit, pancreatic issue that’s not my topic right now. Para, that’s not my topic. Oh yeah, pituitary is MEN-1. 03:45 Pituitary, what’s the most common adenoma, functioning adenoma that you would have in the pituitary? A prolactinoma, good. It’s an acidophil. Here comes the prolactin. 03:56 Okay, good. How is your female presenting? Actually, let’s do the male. How is your male presenting? Decreased libido, decreased sexuality. Why? Because the prolactin is then going to have what kind of effect on your GnRH please? Oh yeah, that’s it. 04:14 So, I’m decreasing my GnRH, inhibiting it. Welcome to secondary hypogonadism. 04:21 Welcome to hypogonadotropic hypogonadism. This is male. Just to make sure we’re clear. 04:27 In a female, how is she presenting? Sure, decreased libido, decreased sexuality. 04:31 But then, what about her nipples? Galactorrhea, milk coming out. Damage to hypothalamus. Radiation is big, maybe a tumor. Hereditary hemochromatosis from head literally to toe. Hereditary hemochromatosis, iron, iron, iron, iron depositing on everything. 04:52 Be very careful, very careful. Listen. If by chance, you find hypergonadotropic hypogonadism, I said hypergonadotropic hypogonadism, where did iron cause damage? Testis. If it’s hypogonadotropic hypogonadism, where did the iron cause damage? Either hypothalamus or pituitary. Clear? Be very careful with iron. Be very careful with the language. This is where they’ll get you but they won’t get you. You’re too good. 05:26 We have congenital disorder, Kallmann syndrome. I’ll talk to you about this in great detail. 05:31 Let me at least give you this. In Kallmann syndrome, this is secondary. We don’t exactly know why but we do know that GnRH is decreased. In addition, the patient is going to have a hard time smelling, anosmia. Just about no condition apart form Kallmann is going to give you such a picture and idiopathic.
About the Lecture
The lecture Male Hypogonadism by Carlo Raj, MD is from the course Reproductive Hormone Disorders.
Included Quiz Questions
Which statement is INCORRECT?
- Levels of testosterone decrease to 150–500 ng/dL in the 6th decade of life.
- The normal level of testosterone in a male 18–29 years old is 700–1,300 ng/dL.
- In secondary and tertiary hypogonadism, LH/FSH levels are abnormally low.
- Hypogonadism of the aging man is considered primary hypogonadism.
- Secondary hypogonadism is a result of pituitary hypofunction.
What type of hypogonadism is seen in Klinefelter syndrome?
- Primary
- Secondary
- Hypogonadotropic hypogonadism
- Tertiary
- Other
In which of the following do we NOT see a pattern of low testosterone, high FSH, and high LH?
- Unilateral anorchia
- Autoimmune orchitis
- Cyclosporine therapy
- Mumps orchitis
- Genital trauma
Which of the following does NOT cause hypogonadotropic hypogonadism?
- Cyclosporine
- Prolactinoma
- Glucocorticoids
- Opiates
- Leuprolide
Which of the following sometimes presents with hypogonadotropic hypogonadism and other times presents with hypergonadotropic hypogonadism?
- Hemochromatosis
- Cryptorchidism
- Kallmann syndrome
- Klinefelter syndrome
- Prolactinoma
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |