Playlist
Show Playlist
Hide Playlist
Inflammatory Bowel Disease Medication
-
Slides Inflammatory Bowel Disease Medication.pdf
-
Download Lecture Overview
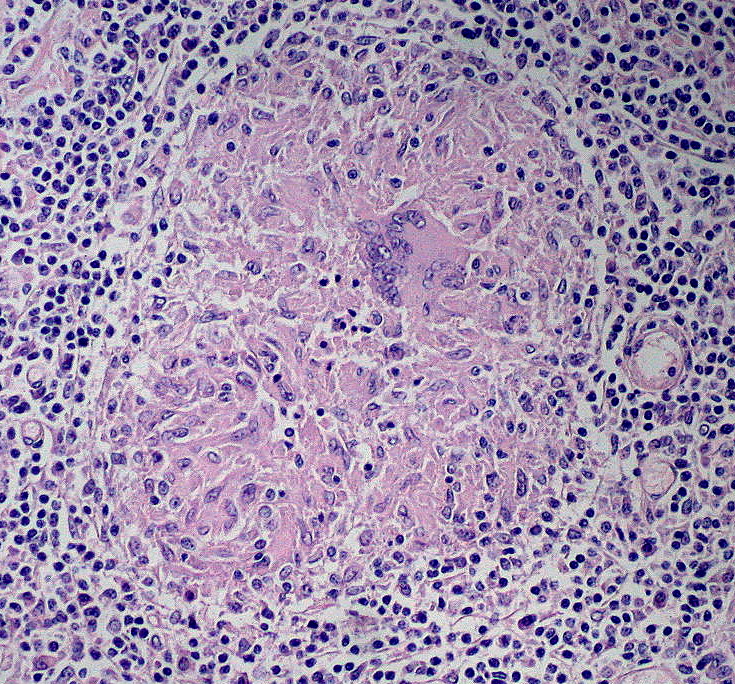
00:01 Welcome to pharmacology by Lecturio. I'm Dr. Pravin Shukle. Today we are going to be talking about the drugs that we use to control inflammatory bowel disease. 00:12 So when we take a look at inflammatory bowel disease, we characterize the disease severity as either mild, moderate or severe. 00:19 And the therapy is going to change based on the severity. So with mild treatment we'll use oral corticosteroids, your budesonide, sometimes we'll use antibiotics or 5-ASA. With moderate disease, we start using biologic agents like the ones mentioned here. And with severe disease, we use surgery and these more aggressive treatments that are listed at the bottom. Now moderate and severe treatments are often similar, but different only in terms of combination therapies or dosing. 00:50 Let's start with mild disease. And let's start with drugs like budesonide and 5-ASA. 00:57 So when we take a look at the way that we treat bowel disease, especially inflammatory bowel disease, we talk about targeting the areas that are affected. So, depending on whether or not patients have Crohn's versus ulcerative colitis, we're going to change the location of where the drugs are, even though the drugs are the same. 01:17 So 5-ASA is a topical therapy in the sense that you take it orally, but it acts topically on the bowel and does not get absorbed. So that's what we mean by topical. We don't mean applying it to the skin. 01:29 These precise mechanisms are really not fully understood in terms of treating inflammatory bowel disease. 01:36 We suspect that leukotrienes are affected by 5-ASA. Now, Pentasa is active in the proximal bowel. 01:45 So we tend to use it more for small bowel disease. On the other hand, Asacol is more active in the distal small bowel and in the large intestine. So patients who have things like ulcerative colitis and disease of the small distal bowel or large intestine are given that therapy. Now when we bind 5-ASA with Azo type moieties, we have an activity that is gonna be limited more to the large bowel or colon. 02:14 So, you can see that by targeting the area, we target the disease. So here's another graphic looking at some of the same information, but now we're gonna focus more on the large bowel. So, I've left 5-ASA regular on there just for illustration purposes. So, balsalazide, gets the mesalazine past the small bowel, and releases it in the large bowel. 02:36 And different formulations will actually work in different parts of the large bowel. Now we also have enemas. 02:43 So rowasa is an enema that is active in the distal colon. So you can see where it fits on the armamentarium. 02:49 And canasa is a suppository that is active in the distal colon and rectum. So like I said, depending on where the disease is, we use different agents. 02:59 Now let's take a look at the antibiotics for mild disease. Now these are used quite commonly despite the fact that we don't have a lot of large scale study supporting its use. We use antibiotics based on biological plausibility. 03:13 And we rely on more anecdotal type of evidence in this type of treatment regimen. It's hard to design a trial to use antibiotics in patients with inflammatory bowel disease because patients are so symptomatic and patients are so sick, that it sometimes becomes unethical to actually commission some of these studies. 03:34 Now we believe that Microbial-derived factors may promote IBD in a susceptible person by disrupting the balance between beneficial and adverse effects of host-microbe interactions in the distal ileum and colon. 03:47 So it seems quite logical and biologically plausible that we would use antibiotics to treat it. 03:54 Let's move on to some corticosteroids. So we also can use topical creams and corticosteroids in proctitis, and they are applied directly to the anal regions and into the rectum. Now budenoside is an oral spray, that is used in respiratory diseases. But we can also administer it as a delayed release pill. And we sometimes use that in inflammatory bowel disease. 04:19 It's used mostly in Crohn's disease involving the ileum or ascending colon. Usually we use about 3 months of therapy. 04:28 We try not to extend past 3 months because then you start to get systemic effects of your therapy. 04:36 We also use it sometimes in remission or assisting in remission, in patients who have ulcerative colitis. 04:45 Azathioprine which is also called Imuran as a trade name, is a widely used agent in transplant medicine and autoimmune diseases in general. 04:55 So it makes sense that we would use it for an inflammatory disease of the bowel. Remember that azathioprine is a prodrug for mercaptopurine. We use azathioprine in moderate to severe Crohn's disease, or chronically active milder Crohn's disease. 05:11 We also use it in fistulizing Crohn's disease. By definition, fistulizing Crohn's disease, is at least moderate disease. 05:19 Fistulizing Crohn's disease may not be that terribly symptomatic, but because it's causing fistulas, we want to be more aggressive. Now, the problem with this particular drug is that it's associated with a low risk of lymphoma. 05:34 The causality is uncertain but we do see an association, so, we are very careful with using this drug. 05:42 Azathioprine is also used in children at much lower doses. The side effects do include nausea and vomiting. 05:49 And other uses include rheumatoid arthritis, systemic lupus, and other skin diseases. 05:58 6-mercaptopurine is also used in transplant medicine and autoimmune diseases. It also interferes with nucleic acid synthesis, including the effects on B and T cell function. It's used in moderate to severe chronic Crohn's disease or chronically active Crohn's disease. And once again, the side effect profile is quite similar. 06:18 It will include nausea, vomiting and diarrhoea. 06:26 Methotrexate is an antimetabolite drug, it's an antifolate drug as well. It interferes with nucleic acid synthesis, and the folic acid pathway. Methotrexate is extensively used in cancer chemotherapy. It inhibits dihydrofolate reductase, and we're going to talk about that in another lecture. This drug is relatively underused in Crohn's disease, but it's important to know for your exams, and I think that we will start to see it used more and more, even though it's an older drug. 06:58 Remember that folic acid supplementation is required for patients who are taking methotrexate. 07:04 So we often give folic acid once a day, and methotrexate is usually given as a single dose, on a once weekly basis. 07:12 Let's move on to another drug called cyclosporine. Now cyclosporine, comes under a variety of names, it can be cyclosporine with an E, or cyclosporine without the E on the end, sometimes it's called cyclosporine A, sometimes it's called Neoral. Now, cyclosporine is metabolized to multiple different isoforms. 07:30 So it can be B, C, D, etc. Metabolites have immunosuppressant activity but are also nephrotoxic. So we have to be very aware of what our cyclosporine levels are. Cyclosporine is extensively used in other diseases as well. 07:44 And it's used a lot in transplant medicine. The problem with cyclosporine is the fact that it interacts with so many drugs, over 2000 drugs interact with cyclosporine. So we have to be constantly aware of the other drugs the patient is on, and we have to constantly check cyclosporine levels, especially when a new drug is being added. 08:05 It becomes even more problematic when people start taking herbal products, virtually every herbal product that actually has a biologic effect will interact with cyclosporine. So it's good to tell your patients not to take any herbal products at all, while they are taking cyclosporine. 08:22 The side effects can include renal dysfunction, it can include tremor, hirsutism, hypertension, gingival hyperplasia, and 30 other side effects of note. You're not going to need to know all of the side effects of cyclosporine, because obviously it's very complex, but what you do need to know it that it is a highly, let's call it a volatile agent in the sense that multiple things can alter its levels, and we do have to check the levels fairly frequently. 08:53 How do cyclosporine A work? Let's talk about its mechanism of action. Let's talk about something called calcineurin. 09:00 So calcineurin is an enzyme in the body. And what it does is it dephosphorylates nuclear factor of activated T cells. 09:10 We call that NF-AT and I'm gonna refer to it several times. So this dephosphorylation causes the transcription of the following agents. Interleukin 2, and the cytokines, okay. Now what cyclosporine does, is it binds to cyclophilin which inhibits calcineurin from activity. So the net effect is, is that you inhibit the production of interleukin 2, and you cause a reduction of the activity of effector T cells, and you reduce cytokines. So that's how cyclosporine A does its job. 09:47 Let's move on to a new class of drugs, called the anti-tumor necrosis factor agents. They are also called TNF antagonists. 09:55 Now these words here, these names of the drugs are virtually unpronounceable, but the most important thing that you want to take from this particular list of drugs is that they all end in -mab. That means that they're monoclonal antibodies. 10:10 Look I said this multiple times in other lectures. The monoclonal antibodies are game changers. 10:16 They're changing everything in medicine, they're turning everything upside down and they're phenomenally effective. 10:22 Let's talk about one of them. Natalizumab is a monoclonal antibody that blocks the integrins on circulating leukocytes. 10:33 So, it may be associated with multifocal leukoencephalopathy, we're not too sure. It's still early in the game, but that's something to be aware off. At this point in time, this very effective therapy is restricted to patients with severe Crohn's disease. And quite frankly we're mostly restricting it to specialists who have experience in this area. 10:55 So general practitioners and general internists aren't really using this medication.
About the Lecture
The lecture Inflammatory Bowel Disease Medication by Pravin Shukle, MD is from the course Gastrointestinal Pharmacology. It contains the following chapters:
- Drugs for Inflammatory Bowel Disease
- Animosalicylates
- Antibiotics
- Corticosteroids
- Antimetabolites
- Cyclosporine
- TNF Antagonists
Included Quiz Questions
What is a common way to classify inflammatory bowel disease?
- Mild, moderate, and severe
- Acute and chronic
- Refractory and sporadic
- Local and systemic
- Antibiotic-sensitive and antibiotic-resistant
What best describes the different formulations of 5-aminosalicylates (5-ASA)?
- The different formulations are administered in distinct ways and target different segments of the bowel.
- The different formulations must be taken as suppositories only.
- The different formulations change the length of time 5-ASA stays in the bowel.
- The different formulations are recognized to be less effective compared to the original product.
- The different formulations are still being developed and are not available for use.
Which drug is associated with a risk of lymphoma?
- Azathioprine
- Anthracycline
- Cyclosporine
- Mesalamine
- Methotrexate
What vitamin must be supplemented in a patient starting methotrexate therapy?
- Folic acid
- Niacin
- Ascorbic acid
- Thiamine
- Vitamin K
Which of the following drugs used in the management of inflammatory bowel disease is classified as a monoclonal antibody?
- Adalimumab
- Azathioprine
- Cyclosporine
- Mesalamine
- Methotrexate
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |