Playlist
Show Playlist
Hide Playlist
Hemostasis – Bleeding Disorders
-
Slides Bleeding disorders.pdf
-
Download Lecture Overview
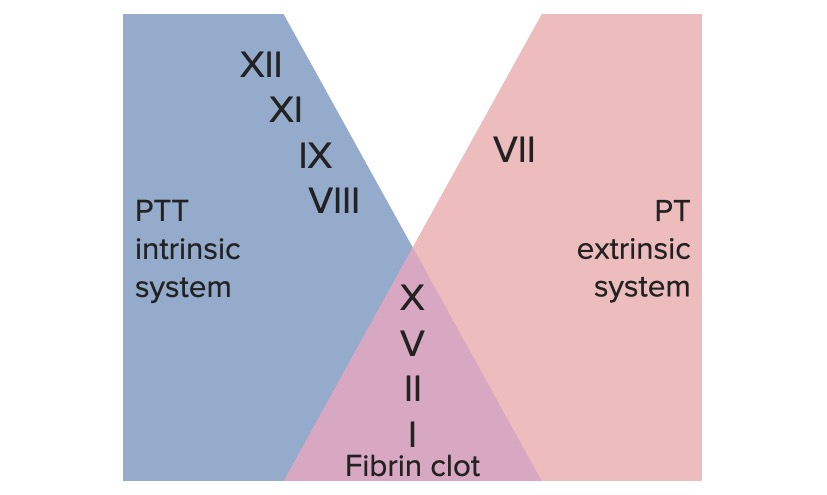
00:01 Hello and welcome to this lecture on bleeding disorders. During this lecture, you will achieve a number of learning outcomes. We will see that hemostasis is dependent on a combined response to injury from the blood vessel, the platelet, and the coagulation system. 00:19 We will see that a range of inherited and acquired disorders can lead to bleeding disorders and we will see that vessel and platelet problems lead to purpura and bruising whereas coagulation deficiency is characterized by bleeds into muscles and joints. When your vessels get injured, a number of processes start. After the initial injury, the vessels can vasoconstrict to reduce the blood flow. Then platelets attach to exposed collagen on the surface of the vessel. These then undergo platelet adherence and an aggregation reaction. We will talk about those in more detail. Finally, coagulation factors ensure that thrombin is generated in order to produce fibrinogen and that stabilizes the clot. This process is really quite remarkable. 01:16 If you prick your finger, you expect that blood to clot within seconds and here we spend most of our life without any problems of inappropriate blood clotting from occasional episodes of thrombosis. 01:31 Let us look at a key player in the system, the platelet. The platelets are shed from the cytoplasm of megakaryocytes. Megakaryocytes live in the bone marrow, the very large cells and they can produce thousands of platelets. On the right, you will see the diagram of a platelet. Besides the platelet is small around three times 0.5 microns and they contain a number of granules. Just look at the main features of the cell. They have that gray canaliculus system. The membrane invaginates into the platelet and provides a very large surface area on which coagulation can take place. The major regulator of platelet production is thrombopoietin and that is produced by the liver and the kidneys and the main function of the platelet is to form a plug on the damaged vessel. You will see another diagram as well, the types of granules the platelet has. Alpha granules containing factors such as platelet derived growth factor, coagulation factors and also the dense granules. 02:53 The platelet response to vessel injury has three major components, adhesion, aggregation, and release. 03:01 And it is important that we go through each of these in more detail. 03:09 Here we have a nice diagram on the right of the platelet in pink adhering to a damaged vessel where the brown represents the exposed collagen on the damaged vessel. On the top right is represented the first process in this reaction platelet adhesion. Look at that blue molecule, that is GPib on the platelet surface and that cross-links through a factor called von Willebrand factor, which binds to the exposed collagen . So that initially draw the platelets to the site of damage. Then another molecule becomes very important. 03:54 You will see right at the top of the diagram is an integrent and is there represented as alpha2b, beta-3. It is also known as GPIIbIIIa; that is how I will refer to it during the next few minutes. GPIIbIIIa gets activated on the amount of this protein has increased on the surface of the platelet. As we move down to the second section, you will see that it is now being involved in cells, binding to von Willebrand factor and to collagen. 04:31 But what happens at the bottom then becomes important. The GPIIbIIIa can crosslink with fibrinogen on the left and von Willebrand factor on the right to draw in more platelets. 04:47 That is the platelet aggregation reaction and then you can see that we formed a primary plug on the damaged vessel. Finally, the platelets get activated and they release the granules into the microenvironment. You will see on the bottom there. The activation leading through a list of ATP and thromboxin and these stimulates the coagulation reaction and they also lead to the platelet swelling in size and forming a more stable plug in the damaged vessel. 05:23 But a platelet plug on its own is not sufficient. It needs to be strengthened by a coagulation cascade leading to fibrin. This is a remarkable system. It is what we called a biological amplification system whereby very small amounts of initiation substances can proteolytically activate a cascade of circulating precursor proteins. It has been estimated the one molecule can lead to the generation of 200 million molecules downstream which I think it makes its remarkable amplification. The key outcome of this is the generation of thrombin, which converts fibrinogen into fibrin and it is this fibrin that enmeshes those platelet aggregates we have just learned about and converts that unstable complex into a stable plug in the vessel. We are going to have to look at the coagulation cascade in a little bit more detail. 06:24 Now, It looks a little complicated. So let us try and make some sense of this. 06:31 Let me take you to the bottom right of that diagram. We have started the bottom and work out, which is little unconventional, but I think it makes some sense and conceive that our aim is to generate fibrin. We need to enmesh the platelet plug to produce fibrin, fibrinogen needs to be activated. For that to be activated we need to generate thrombin from prothrombin and the key enzyme that activates prothrombin is the activated factor Xa. The first of those traditional factor numbers that you may recognize. So there are three proteins, factor Xa, prothrombin, and fibrinogen, which are the core common pathway that we need to remember in this coagulation cascade. Traditionally, we have considered that there are two ways of generating activated factor X. On the top left you will see what was known as the extrinsic system where protein called tissue factor that binds to factor VIIa and activates factor X. On the bottom, it is known as the intrinsic system. We will see factors such as XII, XI, IX being serially activated and leading again to activation of factor X. This has been quite useful because we use common clotting tests to assess these different systems and you will see those represented on all the diagram. In dark blue is the thrombin time, which we will learn later is widely used in medicine, then the bottom activated partial thromboplastin time. Finally for completeness, thrombin generating fibrinogen into fibrin can be measured by the thrombin time. 08:26 But our view of the coagulation system has moved on a little bit and we are trying to update it now to a little slightly different concept. 08:35 Let me take you through this. 08:38 We now think the factor VIIa and tissue factor are critical for the initiation of coagulation. 08:48 There is a small amount of activated factor VIIa in our body. 08:52 It's as if there is a low level of turnover perhaps ready to be fired off when necessary. 08:59 But we now have an updated view of how the clotting cascade may work and the key factors we feel now of factor VIIa and tissue factor. 09:13 Factor VIIa is a very potent molecule. 09:17 But it's thought there are very low levels of activated factor VII around in our blood and whenever there is vascular injury, tissue factor is quickly activated, and binds to VIIa. 09:32 That generates a combination which can do two things. 09:38 In itself, it can generate factor Xa as you see on the right, which remember is one of the critical common pathways to coagulation. 09:49 But also it generates small amounts of factor IXa as well. 09:54 That factor Xa can generate some thrombin, but that is not enough to cause stable coagulation. 10:02 However, thrombin itself can activate three things, which you will see on the diagram: factor VIII, factor V and factor XI. 10:13 These together can provide a huge amplification to this clotting cascade. 10:20 You can see how that happens. 10:22 Factor VIIIa is a cofactor, it is not an enzyme, but it acts with activated IXa to form activated factor X. 10:33 X can then use the cofactor factor Va to activate prothrombin and generate thrombin. 10:43 Then of course we can generate fibrinogen. 10:46 So you can see that the slightly updated view of the clotting cascade provides a mechanism for the initial activation and then the explosive amplification. 10:59 Try and put this together in an overview of hemostasis. 11:04 And just on the left at the top you will see the damage to the vessel wall. 11:08 And what we have to get to is the thing at the bottom, the stable hemostatic plug. 11:15 So after that damage to the vessel wall, we are seeing platelet adhesion through von Willebrand factor and we're also seeing some vasoconstriction. 11:25 The platelet release reaction as well can stimulate the vessel to constrict more strongly. 11:31 That platelet adhesion leads to aggregation and platelet release. 11:37 But we need to trigger the coagulation system as well and that is shown on the right-hand side. 11:43 Tissue factor is the key factor, which activates this leading to a coagulation cascade, which takes place on the platelet granules and on the platelet membrane. 11:58 The coagulation system produces fibrin, which enmeshes that platelet plug and makes the stable hemostatic plug. 12:08 Of course, no biological system can go unchecked and we see on this slide some of the negative regulators of coagulation, protein C and S and antithrombin, and also plasmin, which can break down the fibrin. 12:25 Within the laboratory, we have a number of tests of hemostatic function. 12:30 Of course, the full blood count is the key place to start. 12:33 We need to know the number of platelets within the blood, but clotting tests are also very important. 12:40 There are two that I particularly want to focus on today. 12:43 One is the activated partial thromboplastin time, the APTT and as you will see on the slide, it measures several factors - VIII, IX, XI and VII and normally in the laboratory it takes 30 seconds for blood to clot in this way. 13:02 The second major test that we often do is the prothrombin time or the PT. 13:07 This measures different factors - VII, X, V prothrombin and fibrinogen. 13:12 And this involves a more rapid coagulation 10 to 14 seconds. 13:18 Now you may have heard of this represented as the INR, the International Normalized Ratio and that is where you measure a patient's prothrombin time and you express it as a ratio of a control value in the laboratory. 13:33 And the reason why this is so key is that this is the test we use to monitor warfarin, which is a very common drug, which is given to people with thrombotic problems. 13:45 On the right, we have a table where we see some of the common causes of a prolonged prothrombin time or prolonged APTT. 13:56 So if you look at the prothrombin time, you will see top there is warfarin, which is a drug that we give to the patients with thrombosis. 14:04 We will also see that liver disease and vitamin K deficiency can lead to this test being prolonged. 14:12 Indeed, warfarin is an inhibitor of vitamin K. 14:16 And below that, a disorder called disseminated intravascular coagulation, really a very devastating condition where coagulation is profoundly impaired and then you will see that the APTT and the prothrombin time increased. 14:33 We take the APTT itself, we will see that heparin is the first thing that we put there And indeed, the test was largely developed to test for how much heparin we were giving to patients and to monitor that. 14:49 But critically, it is also increased in hemophilia, a rare but very important disorder as we shall see. 14:57 And again, a range of other conditions as well. 15:00 Finally on the slide on the bottom left, I want to mention the test of platelet aggregometry. 15:08 So we can actually measure in the laboratory how well platelets are able to aggregate in response to factors such as collagen or ADP. 15:18 And in patients with platelet functional abnormalities, that will be suppressed.
About the Lecture
The lecture Hemostasis – Bleeding Disorders by Paul Moss, PhD, OBE, FMed, FRCPath is from the course Hematologic Disorders.
Included Quiz Questions
Which ONE of these is NOT true concerning platelets and their function?
- Platelet nuclei are extruded during the release reaction
- GP1b binds to VWF to promote adhesion
- Platelets bind to exposed collagen on vessels
- Platelets are made from megakaryocytes
- Platelets adhere to each other using the IIb/IIIa receptors
Which of the following molecules is the major regulator of platelet production produced by the kidneys and liver?
- Thrombopoietin
- Thrombospondin
- Thrombogenin
- Thromboglien
- Thrombostatin
Which of the following molecules is involved in platelet adhesion?
- Gp1b
- GpIIb/IIIa
- Fibrinogen
- Factor VII
- GpIb/IX
Which ion is required for the platelet adhesion reaction?
- Calcium
- Potassium
- Sodium
- Chloride
- Iodine
Which of the following factors does not effect aPTT?
- Factor VII
- Factor XII
- Factor XI
- Factor IX
- Factor VIII
Which of the following factors is now thought to be critical to the initiation of coagulation?
- Factor VIIa
- Factor XII
- Factor XI
- Factor IX
- Factor VIII
Which of the following results in the release of granules from platelets?
- Platelet activation
- Platelet degradation
- Platelet synthesis
- Platelet aggregation
- Platelet adhesion
Of the clotting study results shown below, which is most likely to belong a patient with Hemophilia?
- PT - normal aPTT- prolonged Fibrinogen - normal
- PT - prolonged aPTT- prolonged Fibrinogen - low
- PT - prolonged aPTT- normal Fibrinogen - low
- PT - prolonged aPTT- normal Fibrinogen - normal
- PT - normal aPTT- prolonged Fibrinogen - low
Which of the following is strongly associated with PT prolongation?
- Vitamin K deficiency
- Hemophilia
- Von Willebrand Disease
- Lupus anticoagulant
- Heparin use
A 40-year-old female presents with bone pain and gum bleeding. Her CBC reveals leukocytosis. The patient has both a prolonged PT and aPTT with a low fibrinogen. What is the most likely cause of her presentation?
- Disseminated intravascular coagulation (DIC)
- Acute lymphoblastic leukemia
- Amniotic fluid embolism
- HIV infection
- HELLP syndrome
Which of the following is calculated as a ratio of measured prothrombin time to a standard value determined in the laboratory?
- International normalized ratio
- Clotting time
- Activated partial thromboplastin time
- Platelet aggregation time
- Thrombin time
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
2 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like schemas and order of giving material. Easy to use and understand.
very good slides and explanations! Nice voice to listen to