Playlist
Show Playlist
Hide Playlist
Graves' Disease: Treatment – Hyperthyroidism (Thyrotoxicosis)
-
Slides Hyperthyroidism incl. Graves Disease.pdf
-
Download Lecture Overview
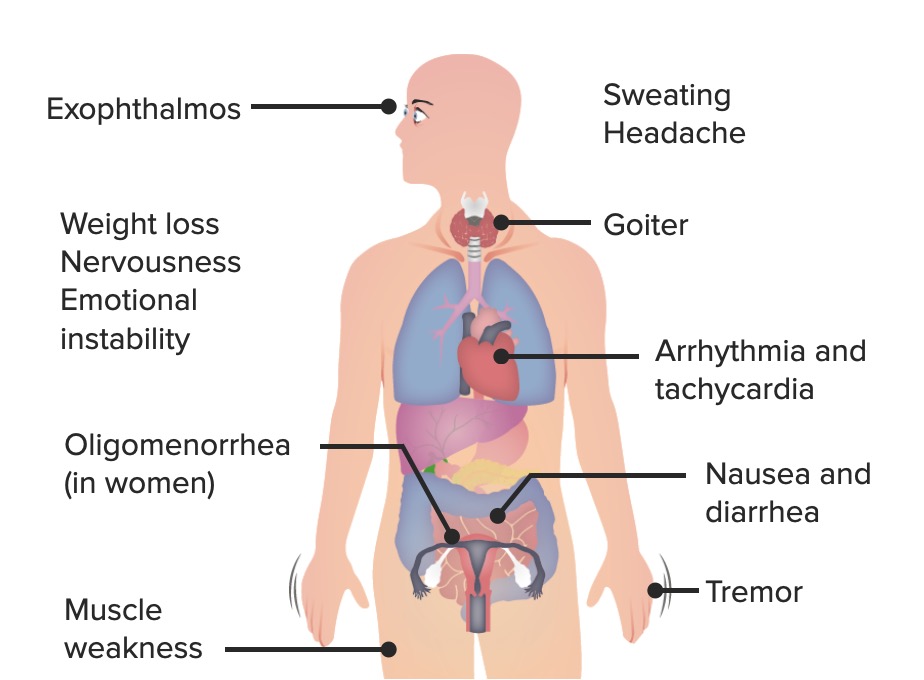
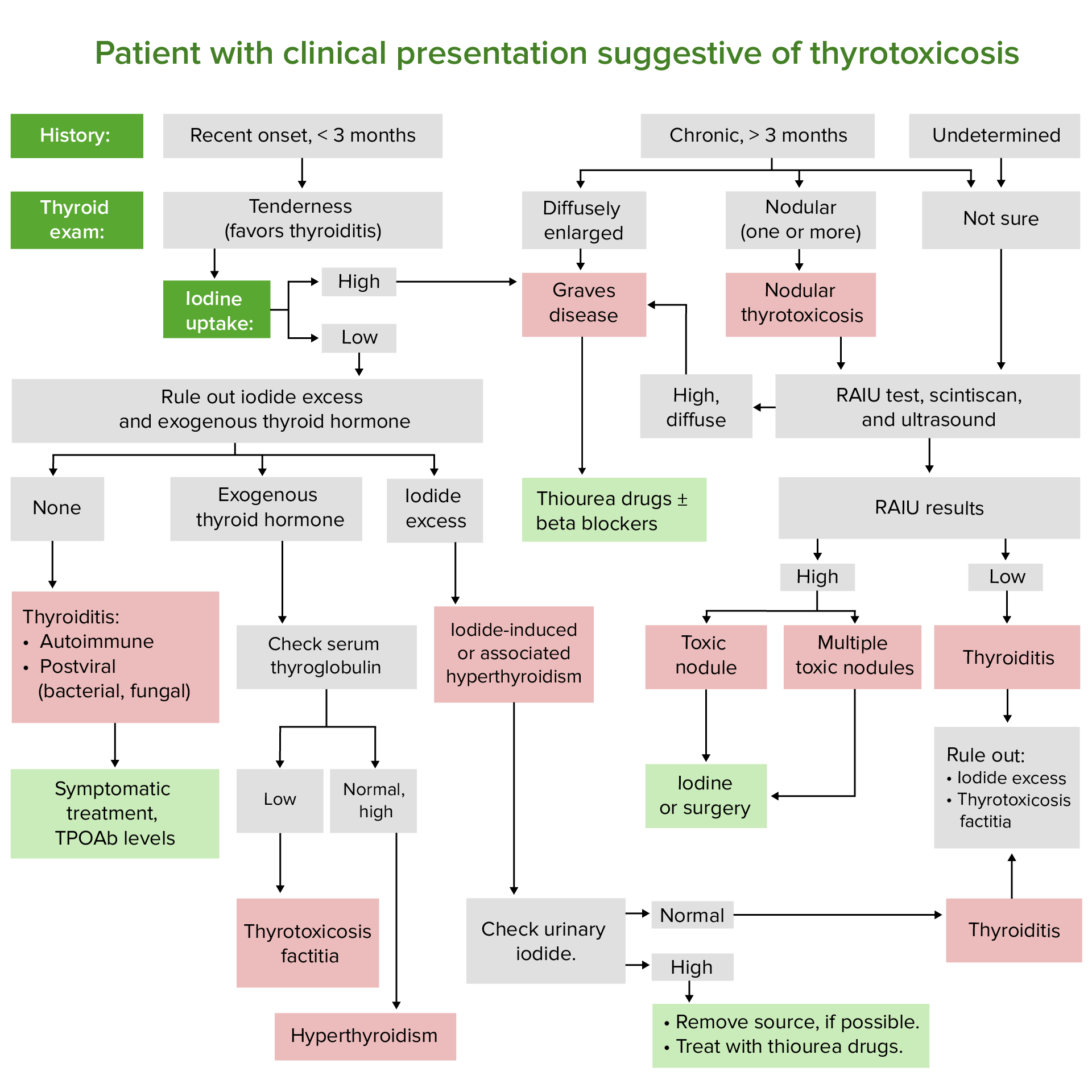
00:01 Let’s talk about management. 00:03 Let’s try to control the symptoms first. 00:06 So, before you do anything, you want to make sure that you’re able to properly regulate the blood pressure and the heart rate in a patient with Graves’ disease. 00:16 With all that T3, T4, you cause increased sensitisation of your catecholamines upon the beta-1 receptor, so it would only make sense that you try to control heart rate and control or manage your palpitations. 00:30 So, you’re looking for drugs that are then going to slow down or block your beta receptors. 00:38 Atenolol or, if it’s non-selective, propranolol. 00:43 Used to control the palpitations. 00:45 “Hey, doc, I feel like my heart is going to jump out of my chest.” Tremors, nervousness, tachy-, anxiety, heat intolerance. 00:53 The ophthalmopathy, local symptoms, how do you control this? Lubricants in the eye drops because it’s like you have all that orbit that’s protruding forward. 01:02 My goodness, it is now exposed to the elements, right? So, therefore, at this point, the lacrimal gland can only take care of what’s normally, you know, controlled by the eyelids, but if it’s exophthalmos symptomatic, be smart about how you manage your patient. 01:20 Take your time. 01:21 Understand what the patient is complaining of and then manage your patient accordingly. 01:26 May require oral steroids, if at all responsive to anti-inflammatory, radiotherapy or perhaps even surgical decompression because you are looking at increased intraocular pressure, aren’t you? So, therefore, it might necessitate some of that decompression that you want to make sure that you address in Graves’ ophthalmopathy. 01:49 Targeting the disease itself. 01:50 So, now, we’ll talk about, apart from symptomatic treatment or management that we discussed earlier, let’s go and start taking care of the thyroid gland. 02:01 Thionamides, inhibits thyroid peroxidase. 02:06 It does not inhibit the release of pre-formed thyroid hormones. 02:09 So, therefore, what has already been formed is formed, but if you inhibit the peroxidase, because back to you understanding of the synthesis of your thyroid hormones, well, all that you’re doing is inhibiting the synthesis of new thyroid hormones. 02:24 What’s been formed has already performed... has already been formed. 02:28 Same concept could also be used with warfarin, right? Warfarin, you cannot take care of the pre-formed coags, but you can sure as heck take the newly synthesised ones. 02:41 Means slow onset, just like warfarin. 02:45 Concept first, then memorise. 02:49 Low incidence of side effects. 02:51 Major, however, side effect would be what’s called reversible agranulocytosis. 02:56 What you’re worried about if a patient is agranulocytic? Susceptibility to infection, rare, but as far as your questions are concerned, whatever may be rare or not, you still want to extremely be aware. 03:12 Rare hepatotoxicity, but could also very much be part of your side effect profile with thionamides. 03:20 What are my thionamides? These include methimazole. 03:24 Drug maintains therapy in non-pregnant patients as once a daily dosing, whereas if you’re thinking about PTU, it’s three time a day (TID). 03:35 Methimazole, associated with aplasia cutis. 03:38 Make sure you know the dermopathologic issue that you find with methimazole. 03:45 PTU, in addition, I pointed this out earlier, in addition to inhibiting peroxidase, which as a general rule of thumb with thionamides, all inhibit the enzyme. 03:58 In addition, PTU will also inhibit the dehydrogenase peripherally so that you’re not able to convert T4 to T3. 04:07 Therefore, all intent purposes you’re trying to manage a patient with Graves’ disease. 04:13 And it’s preferred in pregnancy, as it is less likely to cross the placental barrier. 04:18 So, methimazole, technically, non-pregnant. 04:23 PTU could be used in pregnancy, if needed. 04:29 Remission rate with the drug is less than 50%; best in milder diseases. 04:35 All depends to severity of your Graves’ disease. 04:37 Let’s continue with targeting disease. 04:39 Let’s move away from thionamides with methimazole and PTU. 04:43 Let’s move into radioactive iodine ablative therapy. 04:48 This time, we’re not diagnosing. 04:51 We are in fact ablating or damaging, removing the tissue of the thyroid so that you decrease the production. 05:02 This is what the boards will love. 05:04 You can accidentally remove so much of your thyroid gland that you might then render patient going into hypothyroid. 05:10 Now, that’s an age-old question. 05:12 Just keep that in mind. 05:13 Possibility, sure. 05:15 Hormones, it’s really difficult to control, isn’t it? It is the most common treatment in US for Graves’ disease. 05:19 Iodine is taken into and concentrated in thyroid gland and a single dose treatment, very effective, at complete ablation thyroid function (high cure rate), but works slowly. 05:31 So, here’s the iodine. 05:33 Remember the sodium iodine? That’s important. 05:35 It’ll take it right up. 05:38 It doesn’t know the difference, thyroid gland, does it? But, when it does, it is at that point in Graves’ thyroid which is now being destroyed on purpose with radio-ablative therapy. 05:49 Obviously, this is not the same radio isotope of iodine that you’d use for diagnostic purposes. 05:57 This is for management and treatment, is the ultimate cure, cure. 06:03 Disadvantages – may produce permanent hypothyroidism. 06:08 With enough damage of your Graves’ thyroid gland, you might render your patient into hypothyrotic state. 06:17 Maintain patient on thyroid hormone replacement after radioactive iodine has been given. 06:22 Absolutely contraindicated in pregnancy and breast feeding, for obvious reasons; it’s radiation. 06:29 If by chance you get such a question and for whatever reason there has been radiation exposure by the pregnant woman, then you know that the foetal thyroid is destroyed. 06:39 All kinds of issues. 06:41 May worsen Graves’ ophthalmopathy, especially in smokers. 06:44 Keep that in mind. 06:45 That’s one of those clinical tags that is always added and if you can remember it, that’d be great so that you know as to what’s going on with your patient.
About the Lecture
The lecture Graves' Disease: Treatment – Hyperthyroidism (Thyrotoxicosis) by Carlo Raj, MD is from the course Thyroid Gland Disorders.
Included Quiz Questions
What condition can not be controlled by a β-adrenergic antagonist (e.g., atenolol)?
- Exophthalmos
- Palpitations
- Heat intolerance
- Anxiety
- Tachycardia
What is the mechanism of action of thionamides?
- Inhibition of thyroid peroxidase
- Inhibition of the release of preformed thyroid hormone
- Inhibition of TBG synthesis
- Inhibition of the release of TRH
- Inhibition of the production of TSI
Which adverse effect is associated with methimazole?
- Congenital aplasia cutis
- Hepatotoxicity
- Agranulocytosis
- Gynecomastia
- Hematuria
What is the major adverse event of thionamides?
- Agranulocytosis
- Splenomegaly
- Aplasia cutis
- Alopecia
- Asterixis
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |