Male Repro Review
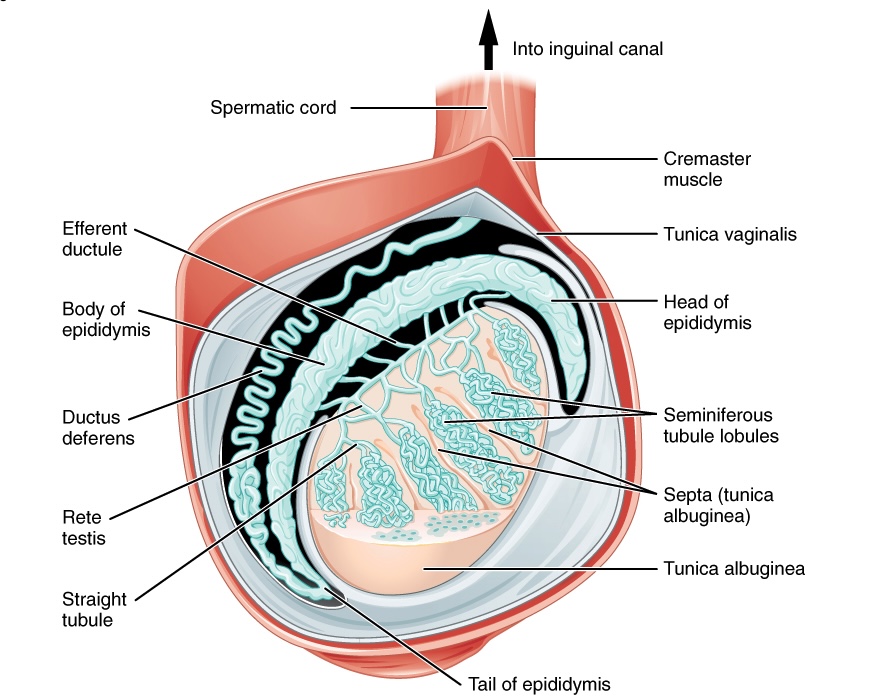
By GLORIA W. on 06. July 2023 for Duct System – Male Reproductive System
Very informative. Brief, to the point. Clear explanation to facilitate understanding.
Histology
By Daniel A. on 17. May 2022 for Reproductive Histology
Too inprecise
In the lecture
You should point out exactly the structures
This doesnt help for exams.
Great presentation, nicely summarised, loved it.
By Pavithra A. on 13. May 2022 for Reproductive Histology
perfectly summarised ,
help us to take a clear outline ,
moreover love presented way..
Awesome
By Aderonke I. on 10. April 2022 for Reproductive Histology
Awesome Professor! Loved the lectures. Great pictures too! Thank you:)
Best histology lectures with physiology guidelines
By yahya s. on 29. August 2021 for Reproductive Histology
Because sir showed diagramatic picture along with histology slide That make it very helpful
Really complete and organized
By Elizabeth A. on 13. May 2021 for Accessory Sex Glands – Male Reproductive System
I chose this rating because I understood the topic easily, thanks to the clear explanations and the organization of the topics
Makes histology so beautiful!
By Favour E. on 20. August 2020 for Reproductive Histology
I really like it, the simplified images makes it quite easy to understand and the slides are well explained. Reasons are given on why the slides look the way they are and how they might appear different from what they really are.
Male Repro
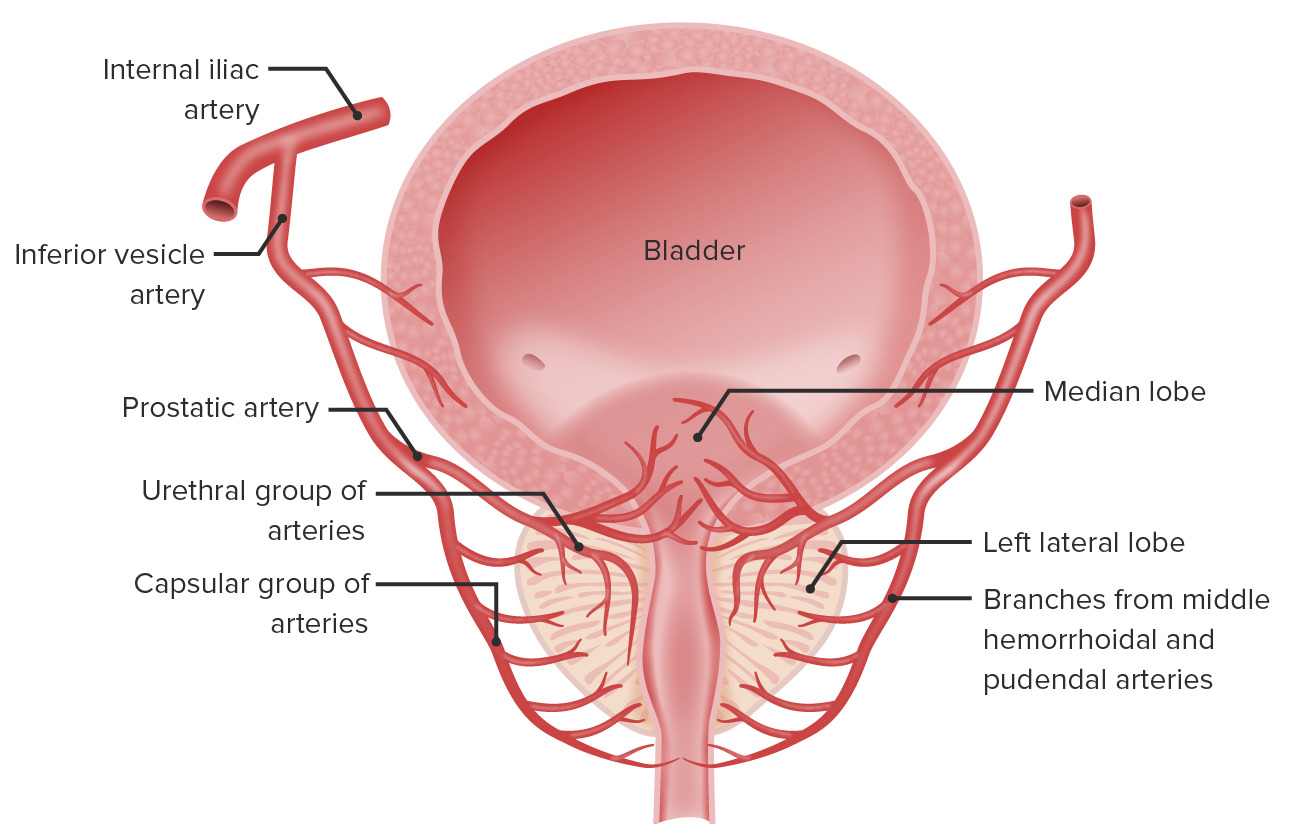
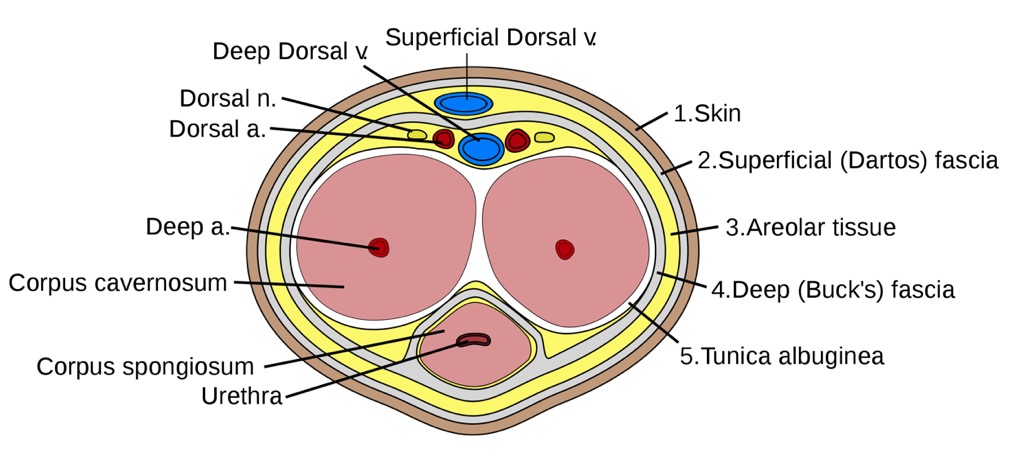
By Catherine C. on 25. June 2020 for Testis: Structure – Male Reproductive System
I really appreciate the labeled pictures. I really helped to understand concepts
Video length
By Erdal B. on 19. April 2020 for Reproductive Histology
The video episodes are way too short, need to go back and start over every 3-4 minutes. I think there should be a option to view the topic in one full video. Otherwise the subjects are well covered in an understandable manner. Many thanks
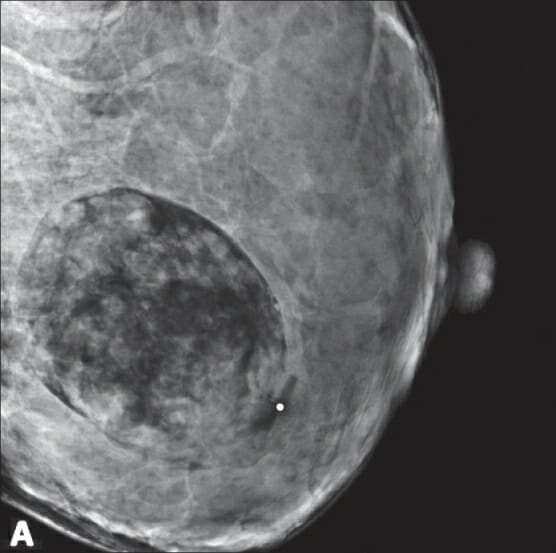
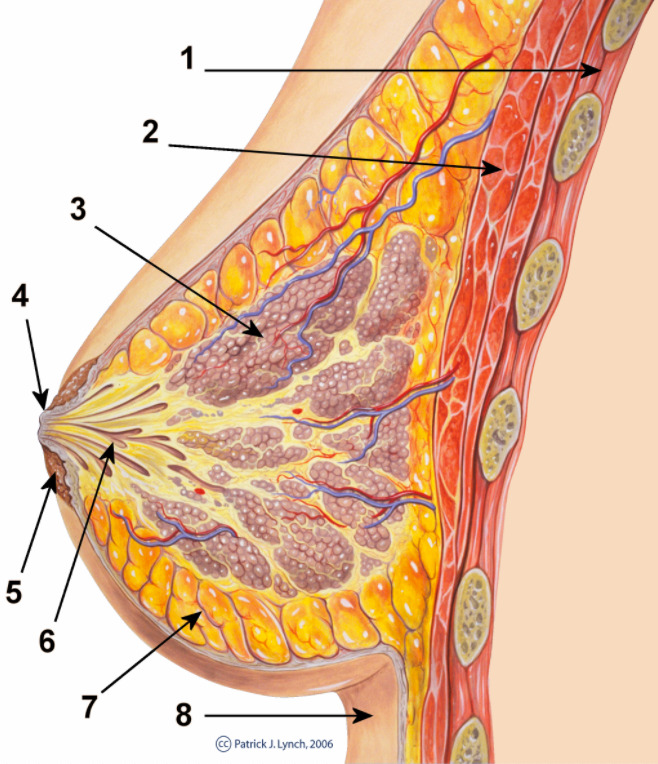
please show what are you talking about
By Mehmet C. on 12. April 2019 for Ovary: Secondary and Mature Follicle – Female Reproductive System
I felt like someone read me a text loudly. It would be much better, if you try to show or point what structure you are talking about. In this way, everything stay as complicated as I read textbook.
Update video graphics
By Sara D. on 17. January 2019 for Ovary: Secondary and Mature Follicle – Female Reproductive System
Its a good lecture but histology is complicated and I wish they would use arrows to point at structures he is talking about instead of just saying look at the right hand side. Or at least put in more labels.
Great!
By Diana C. on 13. January 2019 for Reproductive Histology
Helped to understand everything, and I like the fact that I can speed the video up but still understand it all!!
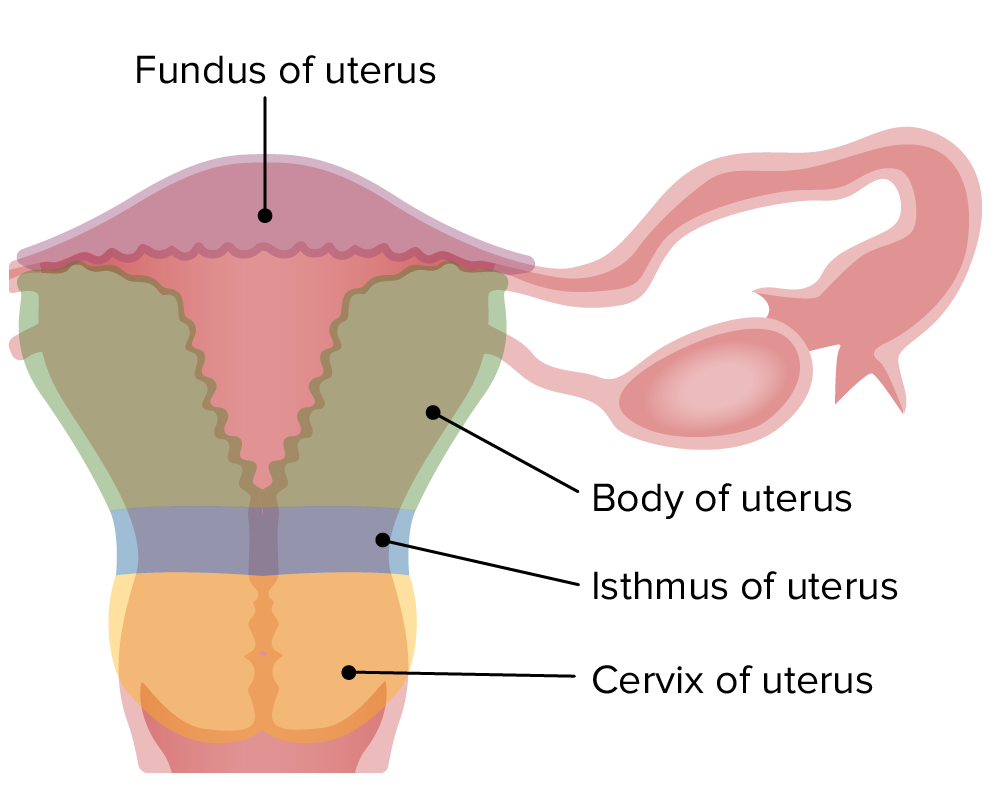
congratulations
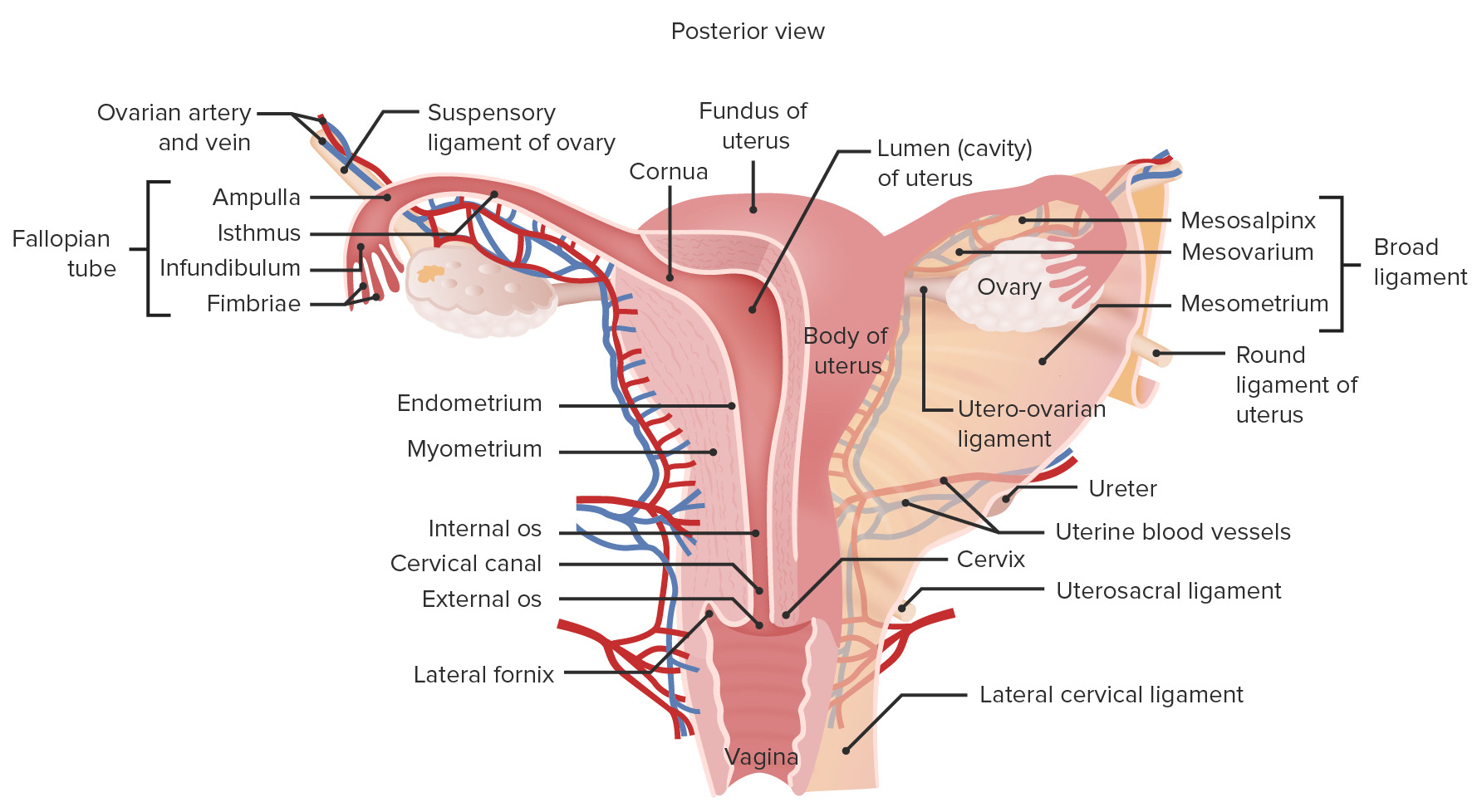
By Alan T. on 13. June 2018 for Ovary: Structure – Female Reproductive System
Absolutely wonderful, the best histology teacher in the world.
I love his classes
a lot of room for improvement
By Christopher G. on 25. April 2018 for Reproductive Histology
the course is histology the guy should at least point to stuff on the histological slides instead of just using a powerpoint. very basic level
Great lecture. Helps a lot!
By Jean-François E. on 13. March 2018 for Ovary: Secondary and Mature Follicle – Female Reproductive System
Great lecture. You make relatively complex notions seem simple. Thank you!
Good
By Perseus M. on 06. December 2017 for Reproductive Histology
Good but not perfect regarding figures and histological slides. I expect more visualized explanation to understand structures than verbal or written explanation