Playlist
Show Playlist
Hide Playlist
Diagnosis of Hypercalcemia and Knowledge Check
-
Slides Hypercalcemia.pdf
-
Download Lecture Overview
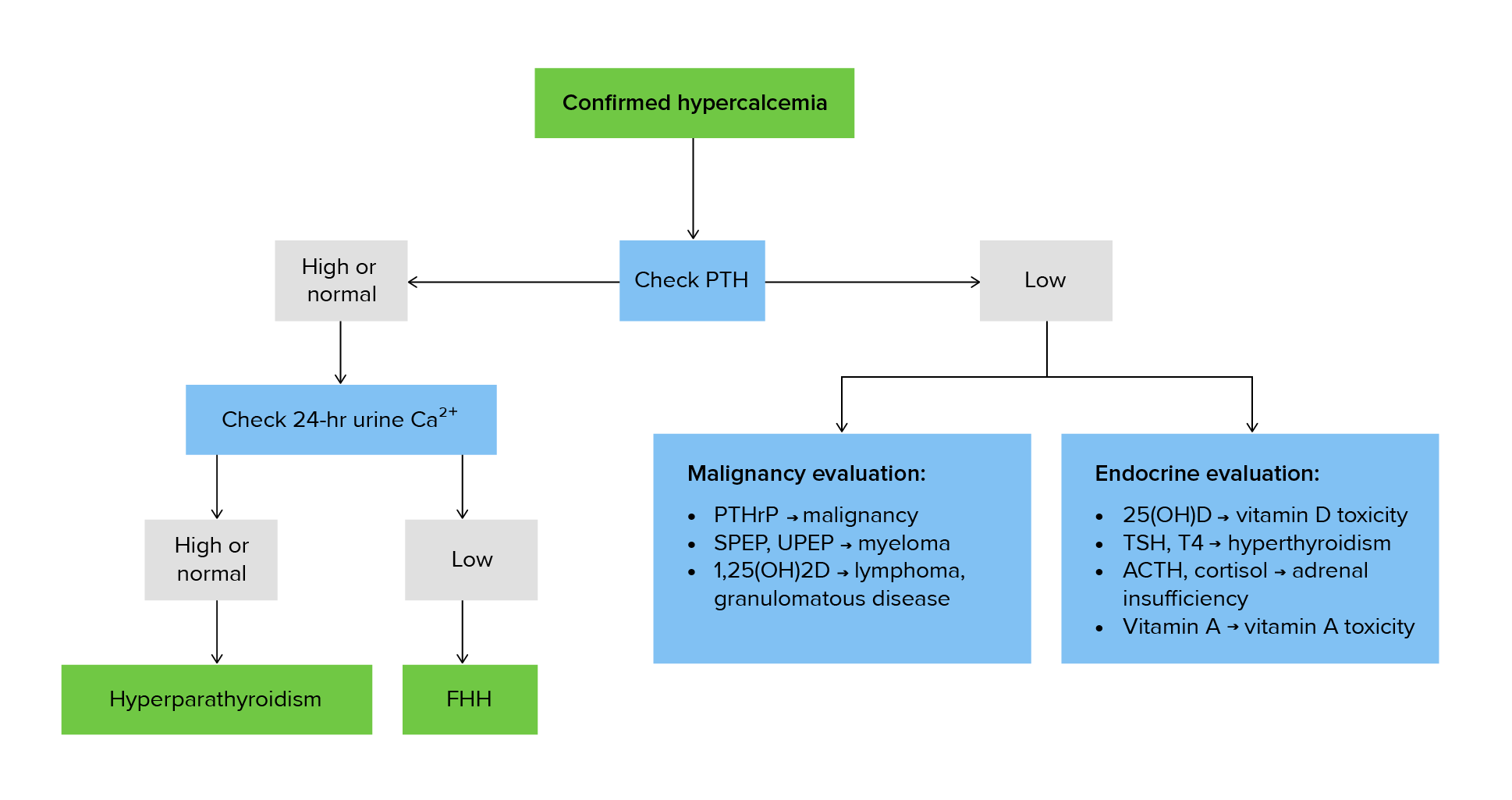
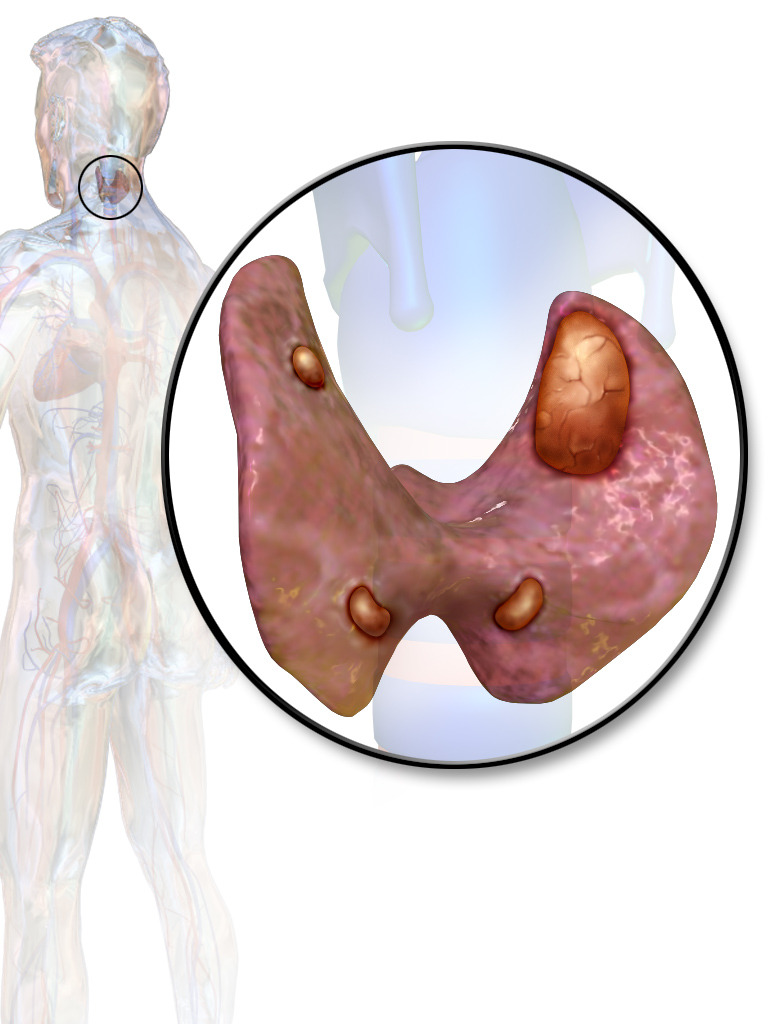
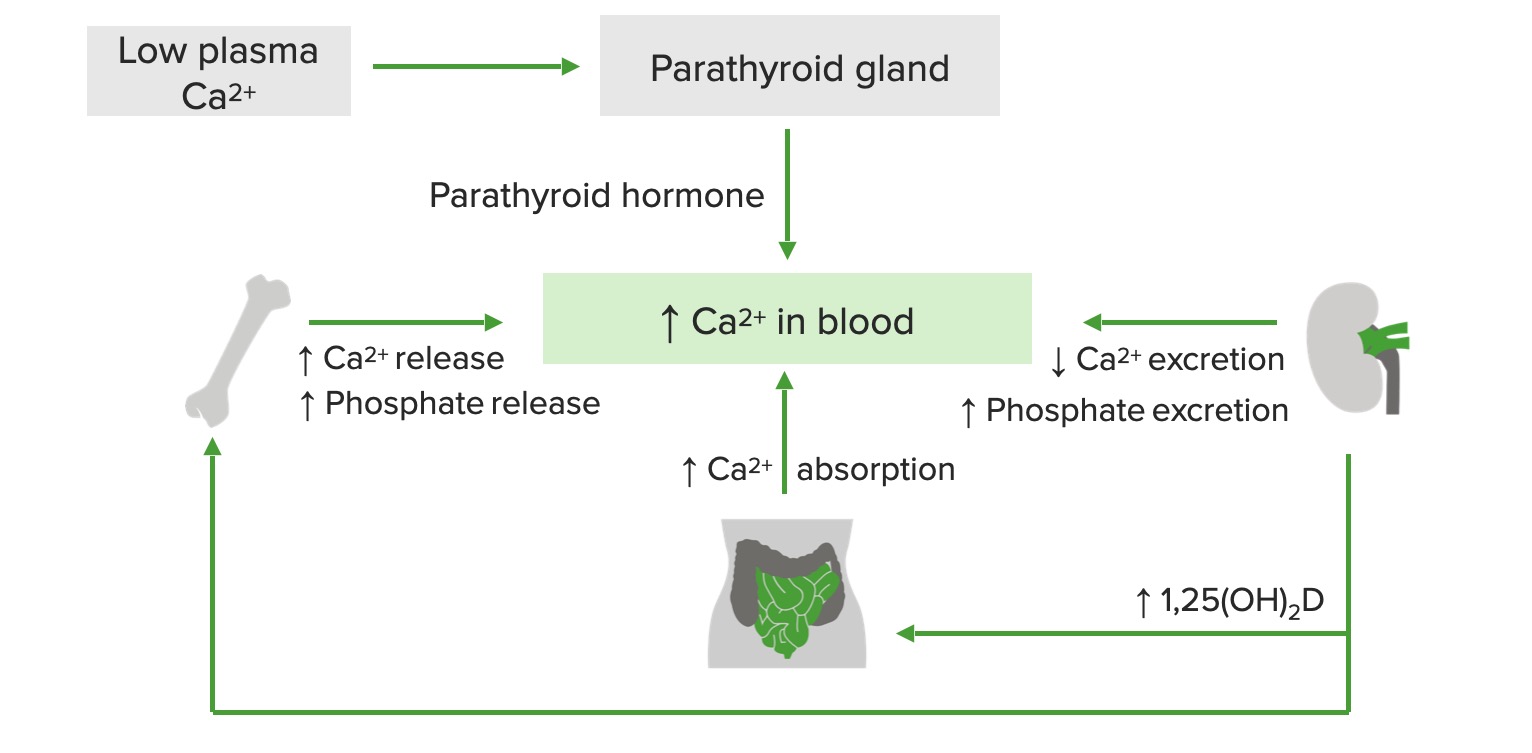
00:01 Let’s take a look at what happens here and I want you to identify some of these patients. 00:06 I’m just going to walk you through a couple. 00:09 We’ll take a look at primary and secondary hyperparathyroidism and that is it. 00:14 Would you please identify, for me, primary hyperparathyroidism? Okay, on your X-axis, we find calcium and on your Y-axis, we find PTH. 00:28 If you have primary hyperparathyroidism, where’s my problem? In the parathyroids. 00:35 And you might have a solitary adenoma, it’s majority of the time will be a solitary adenoma in which it is primarily releasing PTH. 00:43 Next, with all that PTH being elevated, what then happens to your calcium levels? It is also elevated. 00:50 So, which letter here only gives you that exact figure? Let’s take a look at A. A gives you decreased calcium and it gives you high PTH. 01:00 Is that a possibility in primary hyperparathyroidism? I-I am asking you to please identify primary hyperparathyroidism. 01:05 That is not possible with patient A. Patient A with a low calcium may then cause secondary hyperparathyroidism, so we’ve identified that patient. 01:15 Most common cause, renal failure. 01:19 Patient B… Patient B, you find there to be elevated levels of PTH and you also find elevated levels of calcium. 01:26 That’s your patient, ladies and gentlemen, of primary hyperparathyroidism; Patient A secondary hyperparathyroidism. 01:34 You go as far as that, you will be in good shape. 01:38 In this table, we’ll take a look at various diagnosis of hypercalcemia begin by PTH being very high. 01:45 We have primary hyperparathyroidism that we talked about with the solitary nodule, commonly seen with MEN 1 with your pan-pancreas; para-hyperparathyroidism; pit-pituitary, parathyroid-hyperparathyroidism primary. 01:59 2a would be primary hyperparathyroidism; major cancer of the thyroid and pheochromocytoma, if you remember correctly. 02:08 Hypercalcemia, the PTH levels might be normal or slightly high. 02:14 If you find urine and calcium to be depressed and you find hypercalcemia, this may suggest familial hypocalcuric hypercalcemia. 02:26 Understand the concept first, then if you wish, take a look at your values here where we have less than 100 milligrams per day or urinary calcium to Cr ratio of being less than 0.01. 02:39 Otherwise you might be thinking about primary hyperparathyroidism and also… now, lithium is interesting. 02:47 Lithium may then cause hypercalcemia and also, do not forget that lithium may then-then cause damage to your ADH receptors. 02:56 If it cause damage to your V2 receptors, then what do we call this? We call it diabetes insipidus nephrogenic type. 03:04 Okay? So, do not forget about lithium and how it may then cause hypercalcemia, but then may also cause diabetes insipidus. 03:11 We have PTH low or undetectable, but still may result in hypercalcemia. 03:16 What does this mean? Parathyroid function is appropriate for the calcium level. 03:22 Further testing, depending on the clinical picture. 03:24 So, let’s begin. 03:25 You find your PTHrP to be increased, so what does that mean to you? Paraneoplastic. 03:30 Examples, we talked about these squamous cell cancer of the lung and also referred to renal cell carcinoma where you find hypercalcemia, but your PTH levels are low or perhaps even undetectable. 03:44 I mentioned that earlier, make sure that you confirm that properly here for yourself. 03:49 If you find increased levels of 1,25 dihydroxycholecalciferol, maybe it’s granulomatous disease such as your sarcoidosis. 03:57 This may also cause increased levels of calcium which then causes a feedback mechanism where it tells a parathyroid to-to-to shut down or perhaps, there was intoxication of Vitamin D, hypervitaminosis D syndrome. 04:11 Evaluate for thyrotoxicosis; adrenal insufficiency is important as other differentials for hypercalcemia causing a shutdown of your PTH. 04:21 Consider immobilization as well and evaluate for bone metastasis. 04:25 That’s incredibly important.
About the Lecture
The lecture Diagnosis of Hypercalcemia and Knowledge Check by Carlo Raj, MD is from the course Parathyroid Gland Disorders.
Included Quiz Questions
What lab values would be expected in primary hyperparathyroidism?
- High PTH, high calcium, normal to low phosphate
- High PTH, high calcium, high phosphate
- High PTH, low calcium, normal to high phosphate
- Low PTH, high calcium, low phosphate
- Low PTH, low calcium, low phosphate
A patient with hypercalcemia and a normal PTH level has less than 100mg/day of urinary calcium. What is the most likely diagnosis?
- Familial hypocalciuric hypercalcemia
- Primary hyperparathyroidism
- Multiple endocrine neoplasias 2A
- Lithium overdose
- Vitamin D intoxication
What is a specific characteristic of a paraneoplastic syndrome?
- Increased PTHrP
- Increased PTH
- Decreased calcium
- Increased vitamin D
- Urinary calcium < 100mg/day
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |