Playlist
Show Playlist
Hide Playlist
Introduction to Cushing’s Syndrome – Adrenal Gland
-
Slides CortisolHypercortisolism EndocrinePathology.pdf
-
Download Lecture Overview
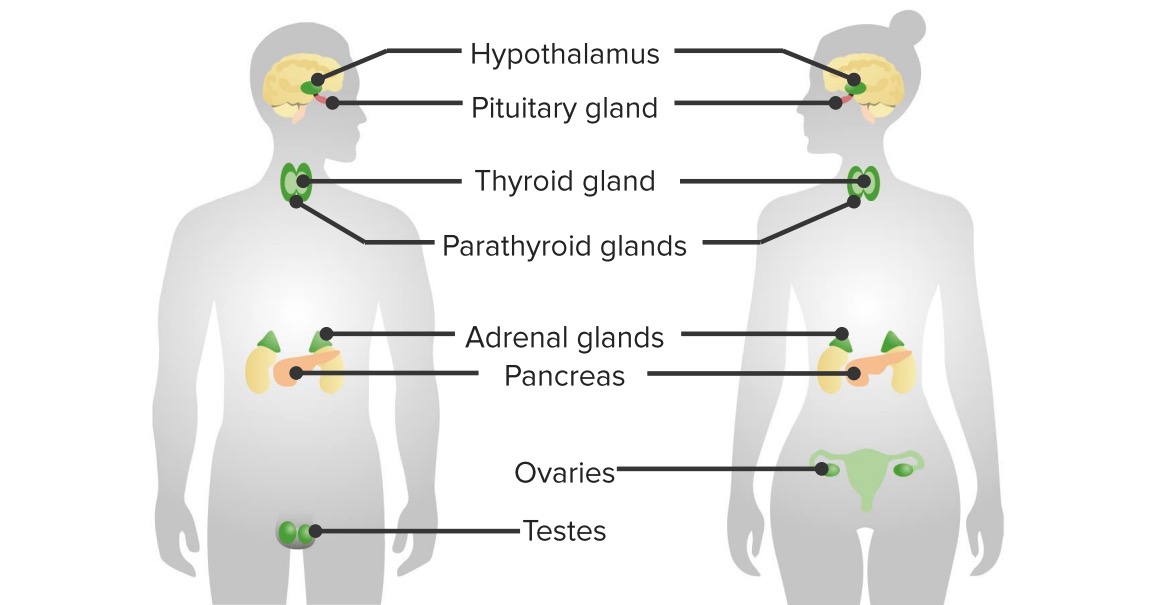
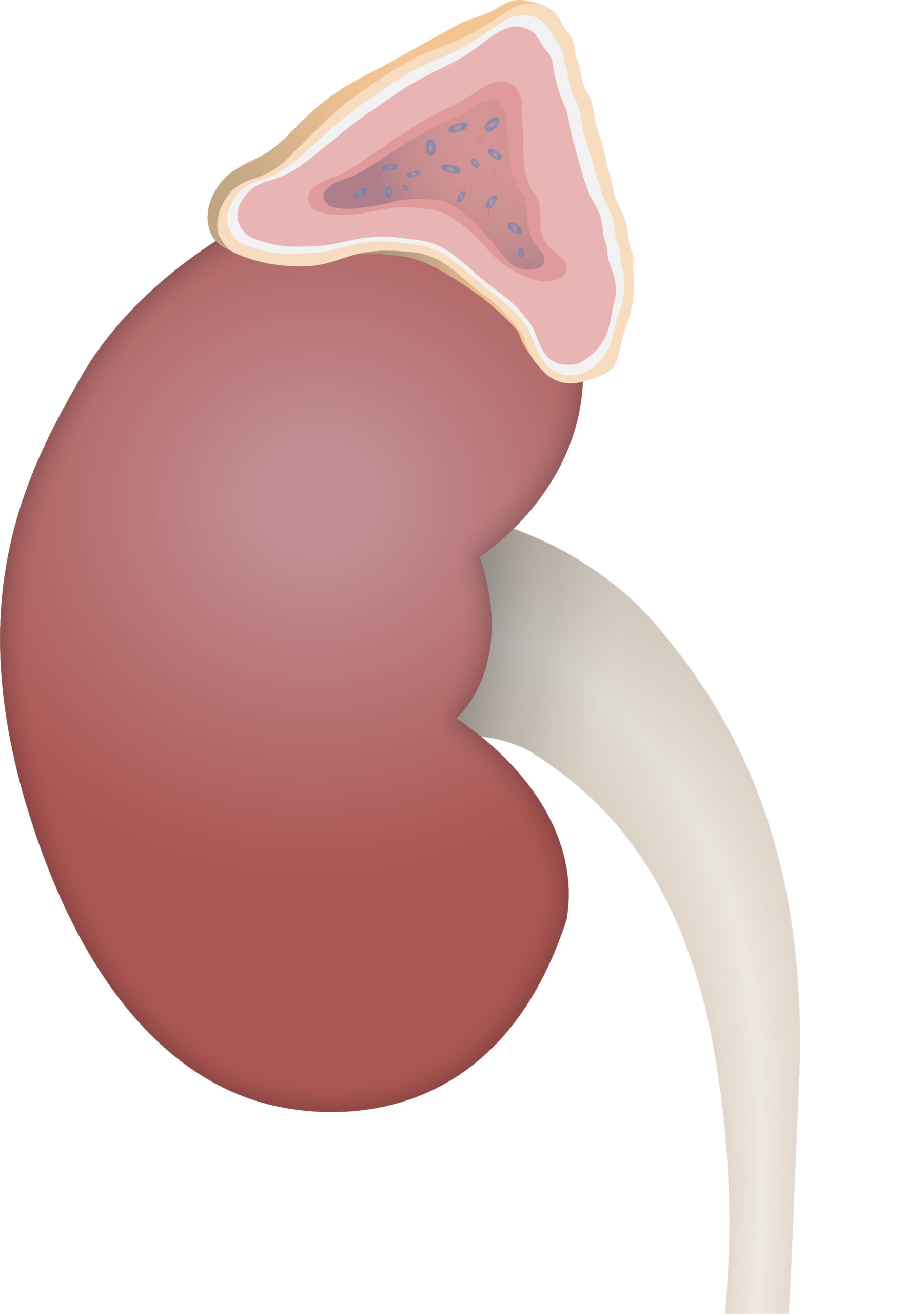
00:02 Let’s first take a look at our first spectrum of pathology here with cortisol and this brings us to, and I’m going to be very specific here, this is Cushing’s syndrome. 00:14 What part of this is specific? The syndrome versus disease. 00:20 Yes, there are two different diagnosis. 00:22 Well, by that I mean, the diagnosis is hypercortisolism for both syndrome and disease, but then disease and syndrome will tell you how cortisol is being-being excessively created. 00:38 Who’s your patient with Cushing’s syndrome in general? Central obesity, because of that obesity, you’ll notice the purple striae. 00:47 What’s striae mean? Stretching of the skin. 00:50 You take a look at the face, looks like a puffy moon facies, facial plethora; acne; hirsutism. 01:02 Understand that Cushing syndrome, if it is being developed as a pathology in the adrenal cortex, would increase all of your adrenocortical hormones. 01:13 Is that clear? So, you will be increasing your aldosterone, you will be increasing, as our topic refers to cortisol, and also increases your androgen. 01:27 What’s hirsutism mean? Hair-like or man-like hair distribution and acne all part of increased androgen, right, androgen production. 01:40 Cervico-dorsal fat accumulation, this is then referred to… take a look at your patient in the area by the trapezius on the neck region, that’s your buffalo hump. 01:51 Easy bruising, thinned skin; muscle wasting especially of the extremities. 01:58 You cannot ever miss a picture of a patient that has excessive cortisol. 02:04 Welcome to hypercortisolism, here we have Cushing’s syndrome. 02:07 Before we move on, you will be responsible for four different places or four different methods by which your patient is going to increase cortisol levels. 02:19 The most common in the US, iatrogenic we’ll talk about; number two maybe from the adrenal cortex; number three from the anterior pituitary producing too much ACTH and that would be Cushing’s disease. 02:36 Paraneoplastically, in the chest, there’s a lung cancer known as small cell lung cancer that may result in ACTH thus cortisol… four. 02:46 If you’re not familiar with all four, not to worry, we’ll go through all of them, all I’m doing is laying down a foundation. 02:55 In addition with Cushing’s syndrome, I told you earlier that not only would you have excess cortisol, but you could have also excess aldosterone… welcome to hypertension. 03:05 Because of excess cortisol, you are then going to have insulin resistance thus diabetes, osteoporosis, immunosuppression, talked to you about lymphopenia. 03:19 There will be proximal weakness specific compared with other signs and symptoms… proximal weakness. 03:26 There will be abdominal striae due to that central obesity. 03:30 Take a look at your patient here and psychological symptoms may also be associated with Cushing’s. 03:38 Once again from head to toe, mental change in hunger, hypertension… why the diabetes? You have diabetes here because of? Good, insulin resistance, glucose intolerance… same language. 03:53 Why the hypokalemia? Good, excess aldosterone. 03:59 How this isn’t Conn’s? This is Cushing. 04:03 My point is in Cushing’s, you’re increasing all adrenocortical hormones. 04:10 Easy bruising, thinning of the skin and striae; thinning of the arms; you have your moon facies, your buffalo hump, your cervicofacial area, increased abdominal fat, trunk obesity, red or purple striae, poor wound healing is a big one and muscle wasting, osteoporosis. 04:32 With Cushing’s syndrome the causes… excess… here we go now, we’ll go through the four. 04:40 Excess glucocorticoids especially cortisol, how? Iatrogenic… iatrogenic would be the most common. 04:47 Now, I want to add a little bit more or at least think… I want you to think about a-a concept that I’m going to offer here. 04:58 If you’re taking a hormone, if you’re taking a hormone, then what does it do to the releasing hormone or the hormone that’s responsible for releasing it? Tell me about the feedback mechanism, you’ll see what I’m getting at. 05:13 Tell me about the feedback mechanism of cortisol. 05:17 Is it renin or is it ACTH? It’s ACTH. 05:20 If you have excess cortisol and you’re giving excess cortisol, what do you think happens to your levels of ACTH? It decreases. 05:35 Keep that in mind, I’m going to keep building on them, building on them, building on them because the language of that-language of that is what the students get confused with. 05:45 Next, more language… slow down, think before you move on. 05:50 ACTH independent, ah, how are you increasing cortisol? How are you increasing cortisol if it’s ACTH independent? Is it in the-Is it in the adrenal cortex, is it in the anterior pituitary, is it in the lung from small cell lung cancer or is it iatrogenic, if it’s ACTH independent? So, if it’s iatrogenic, that’s easy, all that you’re looking for there is in a hospital setting, the doctor might be giving your patient cortisol… iatrogenic, so rule that out. 06:22 First and foremost, that’s the most common. 06:24 Is that clear? Anytime you deal with Cushing’s on exam or anytime a doctor asks you about Cushing’s, you should be ruling out iatrogenic, number one. 06:34 Now beyond that, let’s talk about in vivo, in the body. 06:38 If it’s ACTH independent, how are you increasing cortisol? Good, adrenal cortex, it has to be because if it was ACTH dependent then you might be thinking about anterior pituitary. 06:53 This remind you would be called what? Take a look at the very end here, we have Cushing’s disease. 07:00 So, Cushing’s disease is specific for excess cortisol due to excess ACTH coming from where? What do you mean coming from where? Coming from small cell lung cancer or anterior pituitary? Good, anterior pituitary. 07:16 Do you see how specific the term disease is? What’s syndrome mean? All syndrome means is hypercortisolism, but you don’t know where it might be coming from. 07:28 It could be-It could be one of the differentials. 07:31 Another ACTH dependent condition, the fourth and final one here, and I’ll summarize them again once we’re done, would be perhaps paraneoplastic ectopically and we’re dealing with a particular bronchogenic lung cancer called small cell-small cell lung cancer; not squamous cell, but small cell. 07:50 Find a way to memorize small cell/ACTH; ACTH dependent/ Cushing’s syndrome. 08:01 Four different causes of hypercortisolism… iatrogenic, ACTH independent, that’s cortisol coming directly out of your adrenal cortex; two, ACTH dependent, this being either from the anterior pituitary or from small cell lung cancer. 08:20 Now, we can move on. 08:23 Stepwise approach, what are you going to do? First and foremost, exclude and rule out is your patient somehow getting the cortisol from exogenous use… iatrogenic, factitious. 08:36 It all means the same thing. 08:38 Iatrogenic, factitious, exogenous all means iatrogenic cortisol. 08:43 Know the language. 08:44 Next, we’re going to screen for endogenous. 08:48 In your head, three different places were or three different methods, but you might have hypercortisolism real quick… adrenals, anterior pituitary, small cell lung cancer. 08:58 So, let’s screen for it. 09:01 Do not proceed with workup until… what do you mean by biochemical? Whenever that you can from henceforth on any exam or in a hospital setting on the wards or on the boards, you’ll be always-you’ll be always trying to check for biochemical test or biochemical diagnosis because it’s cheap and it’s effective. 09:22 You don’t want to just order a CT every single time, that is thousands of dollars for you, well, for the hospital, maybe perhaps for the patient and maybe your job, okay? So, this is no joke. 09:34 What kind of biochemical hormone would you be looking for? ACTH. 09:40 Next thing that you want to do is keep separate ACTH dependent causes and ACTH independent causes of hypercortisolism. 09:50 Now, let’s move on. 09:55 Is there hypercortisolism, yes or no? We’ll perform a screen test. 09:58 24 hour urine free cortisol, 1 milligram overnight dexamethasone suppression test. 10:04 Let’s stop there and even to this day, you’re still responsible to knowing the dexamethasone suppression test because of its amazing concept. 10:14 And then I’ll give you a little bit more information as we get to the end of this section in which I’ll give you more current day practice of what you, as a doctor, will be doing in practice, okay? But, let’s make sure that you get your questions right so that you can get into practice. 10:30 We’ll begin. 10:32 Is there hypercortisolism? Okay, now, close your eyes, think about that diurnal pattern that I was telling you about with cortisol. 10:39 When is cortisol the highest? Oh, yeah, in the morning. 10:43 When is it the lowest? At night. 10:45 Next, what’s my feedback mechanism for cortisol? Is it renin or ACTH? Good, ACTH. 10:53 You’re going to give dexamethasone from now on, think of dexamethasone the same as cortisol please, it’s analogous. 11:03 When are you giving this? At night. 11:06 So, you’re going to give cortisol dexamethasone at night. 11:11 Slow down here, work with me. 11:13 If you give cortisol at night, what are you going to do with ACTH levels? Feedback, you should, in a normal patient, decrease your ACTH because you’re giving dexamethasone at night. 11:28 So, wake up in the morning in a normal individual; if you don’t have the ACTH, how much cortisol are you going to have in the morning normally? It should be decreased. 11:38 Hmm, so, now, you give dexamethasone at night, you wake up in the morning. 11:43 Oh my goodness, you find your cortisol to be elevated. 11:46 All that you know now about your patient is hypercortisolism. 11:49 What did you already do before this? Good, you’ve ruled out iatrogenic already, you already ruled out iatrogenic. 11:56 Now, you know is that you have hypercortisolism, three different possibilities. 12:01 So, what’s your next step? Biochemical, biochemical, biochemical. 12:06 So, you’re thinking about ACTH, so it’s either ACTH dependent or ACTH independent. 12:12 Let’s take a look at the algorithm here. 12:14 You take a look at your cortisol level. 12:16 We obviously will be dealing with the elevated branch. 12:18 Let’s do an ACTH level, slow it down, think through this. 12:24 Once you think through it, you’ll be going through this quicker, trust me. 12:28 ACTH level, you find it to be decreased, you find your ACTH levels to be decreased, then where is this hypercortisolism coming from? Good, it’s coming from your adrenals. 12:42 What’s your next step of management? What’s your next step of management? Imaging, maybe CT of the abdomen. 12:50 Not the chest, right? Be careful. 12:53 They might put that, they might put CT of the chest, they might put CT of the abdomen, be smart. 12:58 If your ACTH is to be decreased, that means that the hypercortisolism is being caused by most likely a tumour in the adrenal cortex producing cortisol independently. 13:07 So, this is ACTH independent. 13:10 What’s your next step of management? Imaging of your abdomen to look for that adenoma. 13:17 Okay, so, now, we knocked out two… iatrogenic, we just discussed ACTH independent. 13:25 We’re left with two more, what are they? ACTH dependent. 13:30 Let’s go over to the right aspect of this algorithm please and you find your ACTH to be increased. 13:36 What are the two dependent differentials? Maybe the anterior pituitary or maybe the ectopic small cell lung cancer, right? What are you going to do next? So, where is the excess cortisol coming from? Is it adrenal, is it pituitary, is it ectopic? If you find decreased ACTH, then you’re thinking about your imaging study and you’re dealing with your adrenals. 14:02 If you’re dealing with ACTH, that’s increased, there are two possibilities. 14:06 Now, you do a high dose dexamethasone suppression list. 14:10 Do not, for your boards, worry about the dosage. 14:14 We have low dose and we have high dose. 14:17 So far, what kind of dose will you use? Low, low, low and that I showed you was 1 milligram. 14:25 What about the high dose? Well, the high dose, once again here, do not worry about. 14:30 There are many theories out there as to how it goes by suppressing this, but we’re going to follow the same methodology that we did earlier in the beginning of the algorithm. 14:39 So, let’s give high dose at night. 14:43 You give high dose at night, unbelievably you wake up in the morning and you find your cortisol levels to be low. 14:51 Oh wow, what’s your diagnosis? Good, that’s Cushing’s disease. 14:57 So, for reasons that you must accept from me right now is that high dose dexamethasone suppression test will decrease the ACTH from your pituitary, what’s your next step of management? Imaging, MRI of what? The head. 15:13 What are you looking for? An adenoma in the pituitary releasing ACTH. 15:19 This is secondary hypercortisolism. 15:21 Are you with me? Lot of information here, it is most important that you keep things organized. 15:28 If you feel yourself right now losing morale and you’re feeling frustrated, pause me for a second, go back from the top and go through step by step by step of this algorithm so you’re perfectly clear with the organization. 15:43 You do this a few times, you’ll be like a record and you’ll be doing it automatically. 15:48 Let’s do another one. 15:50 So, we do high dose dexamethasone suppression test, but this time you don’t suppress the ACTH, you don’t. 15:55 What’s your next step of management? Chest X-ray, okay? Chest X-ray. 16:02 What are you looking for? You’re looking for a primary nodule by the mediastinum most likely being caused by small cell lung cancer. 16:11 What’s your next step of management after that? That’s more-more of a step two CK, isn’t it? But, you already know, surgery. 16:20 There are a lot of questions that are coming down from step two CK into step one. 16:23 So, next step of management is always important for you. 16:26 So, is the excess cortisol ACTH dependent or is it independent? We already took care of-We already took care of our independent. 16:35 Next, you perform a high dose and that particular dosage is 8 milligrams overnight and we said that if you find your ACTH to be depressed, then your ACTH is coming from your anterior pituitary Cushing’s disease. 16:49 Whereas if it’s not being suppressed, then that ACTH is coming from your small cell lung cancer, perhaps ectopically. 16:57 After confirmation of hypercortisolism, check ACTH. 17:00 ACTH is suppressed, sources likely a cortisol producing… please take a look and pay attention to imaging… abdomen, CT/MRI. 17:10 If ACTH is normal or elevated, perform high dose and we do high dose dexamethasone suppression test and you find your cortisol to be depressed, then you do your next step of management MRI of the pituitary to find an adenoma there. 17:26 If you do not find cortisol suppression, then you’re looking at and you perform a chest X-ray... and this specifically... or a chest CT and consider doing what’s known as an octreotide scan. 17:40 And all of this may then help you diagnose your patient with having small cell lung cancer of the chest.
About the Lecture
The lecture Introduction to Cushing’s Syndrome – Adrenal Gland by Carlo Raj, MD is from the course Adrenal Gland Disorders.
Included Quiz Questions
What is NOT a classic sign of Cushing's syndrome?
- Muscle hypertrophy
- Moon facies
- Cervico-dorsal fat accumulation
- Central obesity
- Easy bruising
What is the mechanism for the development of diabetes mellitus in patients with Cushing's syndrome?
- Insulin resistance secondary to increased cortisol
- Glucose intolerance due to central obesity
- Central obesity leads to insulin resistance
- Increased inflammatory markers leading to insulin resistance
- Decreased gluconeogenesis leading to central obesity
What is the cause of Cushing's disease?
- Pituitary hypersecretion of ACTH
- Iatrogenic
- Adrenal hypersecretion of cortisol
- Ectopic hypersecretion of ACTH
- Ectopic hypersecretion of cortisol
After nighttime administration of 1 mg of dexamethasone, what is considered an abnormal dexamethasone suppression test?
- Increased serum cortisol in the morning
- Decreased serum cortisol in the morning
- Increased serum cortisol at night
- Decreased serum cortisol midday
- Increased serum cortisol midday
Which malignancy is associated with ectopic hypersecretion of ACTH?
- Small cell carcinoma of the lung
- Mucus secreting pancreatic carcinoma
- Adrenal adenoma
- Pituitary hyperplasia
- Clear cell renal carcinoma
What is the most likely diagnosis in a patient with hypercortisolism with suppressed ACTH levels?
- Cortisol-producing adrenal tumor
- Pituitary adenoma
- Mucus secreting pancreatic carcinoma
- Small cell carcinoma of the lung
- Clear cell renal carcinoma
Customer reviews
4,9 of 5 stars
| 5 Stars |
|
6 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Excellent approach of teaching . Hope more lectures on other topics
Excellent! Stepwise approach and use of algorithm very easy to follow. Helped strengthen by a vast amount my pre-existing understanding of this topic.
I need to watch it for 2 times . It is very helpful. Specific information for the exams.
Excellent detail and explanation. Thank you Dr Carlo Raj - Amazing
1 user review without text