Playlist
Show Playlist
Hide Playlist
Cervical Cancer: Pathogenesis
-
Slides Cervix Female Reproductive Pathology.pdf
-
Download Lecture Overview
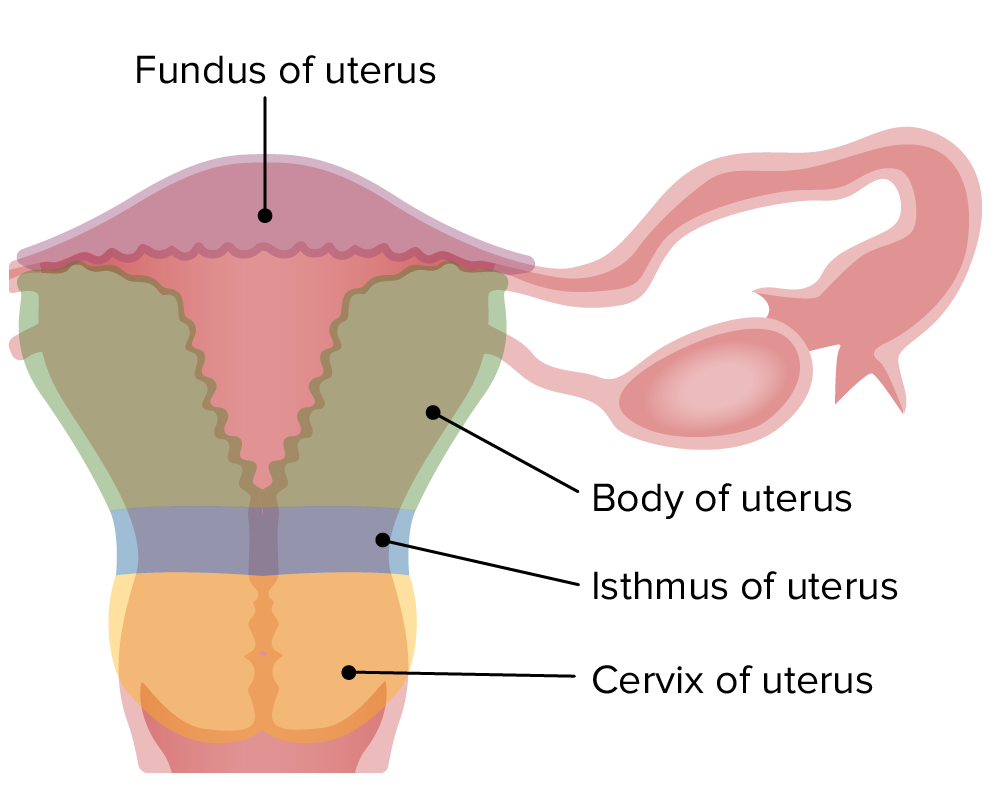
00:01 Pathogenesis of cervical cancer. 00:04 I'll quickly walk you through the algorithm that's important for you. 00:08 You’ve seen this before in some way, shape, or form. 00:11 I like the organization pattern that is being established here for you. 00:15 Sexual activity. 00:17 The more that you have a partner that is promiscuous, then she increases her risk for HPV exposure. 00:26 In basic pathology, we talked about neoplasia. 00:29 In neoplasia, we talked about HPV high-risk strain containing particular oncogenes. 00:35 And those included E6 and E7. 00:38 E6 knocked out p53; E7 knocked out Rb. 00:44 If you knock out the tumor suppressor gene, you are now going to choose a cell in the transformation zone of either becoming an adenocarcinoma or a squamous. 00:55 Your focus will be on the left branch of this algorithm. 01:00 Infection with high-risk HPV is very common, and is seen in up to 80% of sexually active adults before age 50. 01:06 It is transient and clears on its own in majority of the cases. 01:10 Only a few women who have persistent infection may finally develop cervical intraepithelial neoplasia (CIN) or cervical cancer in later years. 01:18 The risk of progression in the high-risk HPV-positive women with a normal cervix or low-grade lesion on colposcopy and histopathology at baseline is not yet clear, but about 10% of women with HPV infection will develop a persistent viral infection that puts them at risk for cervical cancer. 01:35 It is important to know the most common high-risk strains of HPV are 16 and 18. 01:40 Similarly, when high-risk HPV lingers and infects the cells of the vulva, vagina, penis, or anus, it can cause dysplasia. 01:49 So now, you begin the process of dysplasia, and there are three different types. 01:57 CIN 1, CIN 2, CIN 3. 02:00 Cervical intraepithelial neoplasia, CIN 1, 2, 3. 02:07 You go straight to CIN 3. 02:09 Close your eyes. 02:10 What’s happening right now? Dysplasia. 02:12 Dysplasia. 02:13 Can you picture increased proliferation of squamous cells right now? That means that the membrane is getting more -- it’s bearing more and more weight. 02:23 Think of it that way. 02:25 With all this proliferation, the membrane, which is still intact, is now bearing all this weight. 02:31 Oh my goodness. 02:33 At some point, from CIN 3, you’re going to become malignant. 02:38 At this point, what form are you in? You’re in dysplasia. 02:42 That is not a neoplasia. 02:44 It is a dysplasia, but it’s not a cancer. 02:47 It’s not malignant. 02:49 So your next step in terms of malignancy will be in situ. 02:51 And then you’re going to invade. 02:54 If you then invade, you become now invasive cervical cancer. 02:58 Let’s pause here for a second. 03:01 You should be familiar with CIN 1, 2, and 3. 03:03 We’ve talked about it in microbiology. 03:04 I will talk to you about this a little bit more. 03:06 However, clinically, this might be new information for you, that you need to make sure that you’re familiar with. 03:15 You no longer will call this CIN when you document it. 03:19 When you document the changes that you find on Pap smear, okay, you’ve taken a sample of the cell and you’re looking at it now. 03:27 When you document it, you’ll be writing down what type of SIL has been taking place. 03:36 SIL stands for squamous intraepithelial lesion, SIL. 03:41 There is either low grade or high grade. 03:44 Please focus upon high grade SIL. 03:48 What high grade SIL means is the fact that you’re getting step by step by step closer to invasive squamous cancer. 03:58 Here we have the following, high grade and also risk factors that are involved. 04:03 Smoking, oral contraceptive pills, high parity, altered immune status, and maybe perhaps, host gene alterations All of these factors, high grade, you’re increasing risk of? Invasive squamous cancer. 04:21 Take a look at the very left. We have low grade. 04:24 Low grade has a rare chance of going on to invasive squamous cancer. 04:29 Think of this, please, as being like CIN 1. 04:34 Once you go past CIN 1 and you go into CIN 2 and 3, this is your high grade. 04:43 And once again, to high grade, you’ll increase the chance of going on to? Invasive squamous cancer of what organ right now? Cervical. 04:52 How important is this? Worldwide developing countries, cervical invasive cancer is the number one cancer gynecologically. 05:03 What about the other side? On the right branch, what part of the cervix are we in if it’s columnar? Endocervical columnar differentiation. 05:14 If this is endocervical, what kind of cells are these? Good. 05:19 These are columnar cells. 05:21 Therefore, why would you ever call this squamous intraepithelial lesion? That makes no sense. 05:28 You would call this glandular intraepithelial lesion. 05:32 "But Dr. Raj, I’ve never heard of that before." That’s okay, that’s good, because that means that you’ve been taught that majority of your cervical cancer is of what type? Squamous, squamous, squamous. 05:44 Human papillomavirus (HPV) is central to the development of cervical neoplasia and can be detected in 99.7 percent of cervical cancers. 05:53 HPV types 16 and 18 are found in over 70 percent of all cervical cancers, with other high-risk subtypes seen less often. 06:01 The most common histologic types of cervical cancer are squamous cell (70 to 75 percent of the time) and adenocarcinoma (about 25 percent of the time). 06:11 Other rare types are adenosquamous, adenoid cystic, neuroendocrine, mixed, and undifferentiated carcinomas. 06:19 Most abnormalities are treated early with detection on Pap smears and never progress to cervical cancer when patients have regular screening.
About the Lecture
The lecture Cervical Cancer: Pathogenesis by Carlo Raj, MD is from the course Disorders of Vulva, Vagina and Cervix.
Included Quiz Questions
What is the term for the epithelial transformation that occurs in cervical intraepithelial neoplasia?
- Dysplasia
- Metaplasia
- Hyperplasia
- Hypoplasia
- Hypertrophy
In what condition would a Pap smear show mildly dysplastic squamous cells closely resembling normal cells?
- Low-grade squamous intraepithelial lesion (LSIL)
- High-grade squamous intraepithelial lesion (HSIL)
- Squamous carcinoma in situ (CIS)
- Undifferentiated squamous cell carcinoma of the cervix
- Adenocarcinoma of the cervix
In a patient with a high-grade squamous intraepithelial lesion (HSIL), which of the following factors are associated with the risk of malignant transformation?
- HIV infection, high parity, oral contraceptive use, smoking
- Smoking, exposure to chemicals, obesity, pregnancy
- Alcohol consumption, concomitant herpes infection, smoking, intravenous drug use
- Hypertension, obesity, chronic pelvic inflammatory disease
- There is no evidence for any risk factors associated with malignant transformation of squamous intraepithelial lesions.
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
I like how he didn't just read off the slides and was quizzing us throughout! amazing, wish he was my lecturer.