SATISFACTION WITH THE CONTENT
By Deed M. on 27. November 2022 for Airway Diseases
I am enjoying studying here, the contents are well arranged plus the videos and the questions with well explained answers
Maybe about adding up the dosages of drugs plus the page should be staying longer on without internet
Excellent
By Michael N. on 04. June 2022 for Airway Diseases
Prof Brown is just amazing at explaining concepts, I really loved his videos.
So much great information in one location!
By Barbara R. on 31. May 2022 for Airway Diseases
This course is outstanding and great supplemental information for my courses. It’s easy to follow and provides just enough details about each topic concept. A lot of high yield information. I’d highly recommend these courses to any FNP, PA, or Medical students!
Great lecture! (:
By Esmeralda G. on 22. February 2022 for Asthma: Lower Airways Obstruction
Great content, well-explained and the lecture was easy to follow. Thanks!
Useful course
By Niloufar A. on 20. February 2022 for Airway Diseases
Very useful information and specially Dr Brown used UK guidelines was very useful and interesting
good explanation of pathogenesis
By Alaena A. on 08. September 2021 for Asthma: Clinical History
I like the explanation of the pathogenesis and some clarification between allergic and non-allergic asthma.
I don’t appreciate Respiratory lectures.
By Malakamir M. on 04. September 2021 for Airway Diseases
1- The accent of the lecturer is not comprehensive, as if he tried to emphasize on his accent. Instead of TALK, he said TOK is a simple example! I’m sure if he went to the USA, they will say:” Please repeat!” I myself understand a little the British accent, but he didn’t talk only for the British students or MDs. I had to look at the subtitles. I have not this problem with others.
He didn’t use a case problem like a USMLE question to develop his lecture. He simply read what it was in front of him. If I compare the quality of Respiratory lectures with Rheumatology, for example, I can say that I didn’t learn anything.
Airway disease rating
By MOHAMMED S. on 23. May 2021 for Airway Diseases
Dr Jeremy Brown is a very good professor, he has a unique way to make you understand airway diseases.
Since I am a foreigner i find it hard sometimes to understand him so i have to rewind sometimes.
i would recommend this course to any medical student who wants to really understand airway diseases.
Lecture is great
By Irfan A. on 26. March 2021 for Airway Diseases
Love it,love it,love it,love it love it
Question are highly beneficial
By Manindra nath S. on 06. January 2021 for Airway Diseases
Good discussion with picture, it help me to understand.all topic discussion was good.
easy to understand
By hazizslah J. on 21. November 2020 for Chronic Obstructive Pulmonary Disease (COPD): Overview
Very good I like him a lot , I can understand him very easily
Good
By A.A N. on 21. June 2020 for Airway Diseases
Nice session for medical students preparing for final year exams
His technique should be changed if not him.
By Adithya S. on 14. June 2020 for Asthma: Clinical History
The lecturer's way of teaching is bland and his accent is pretty confusing.
Excelent lecture
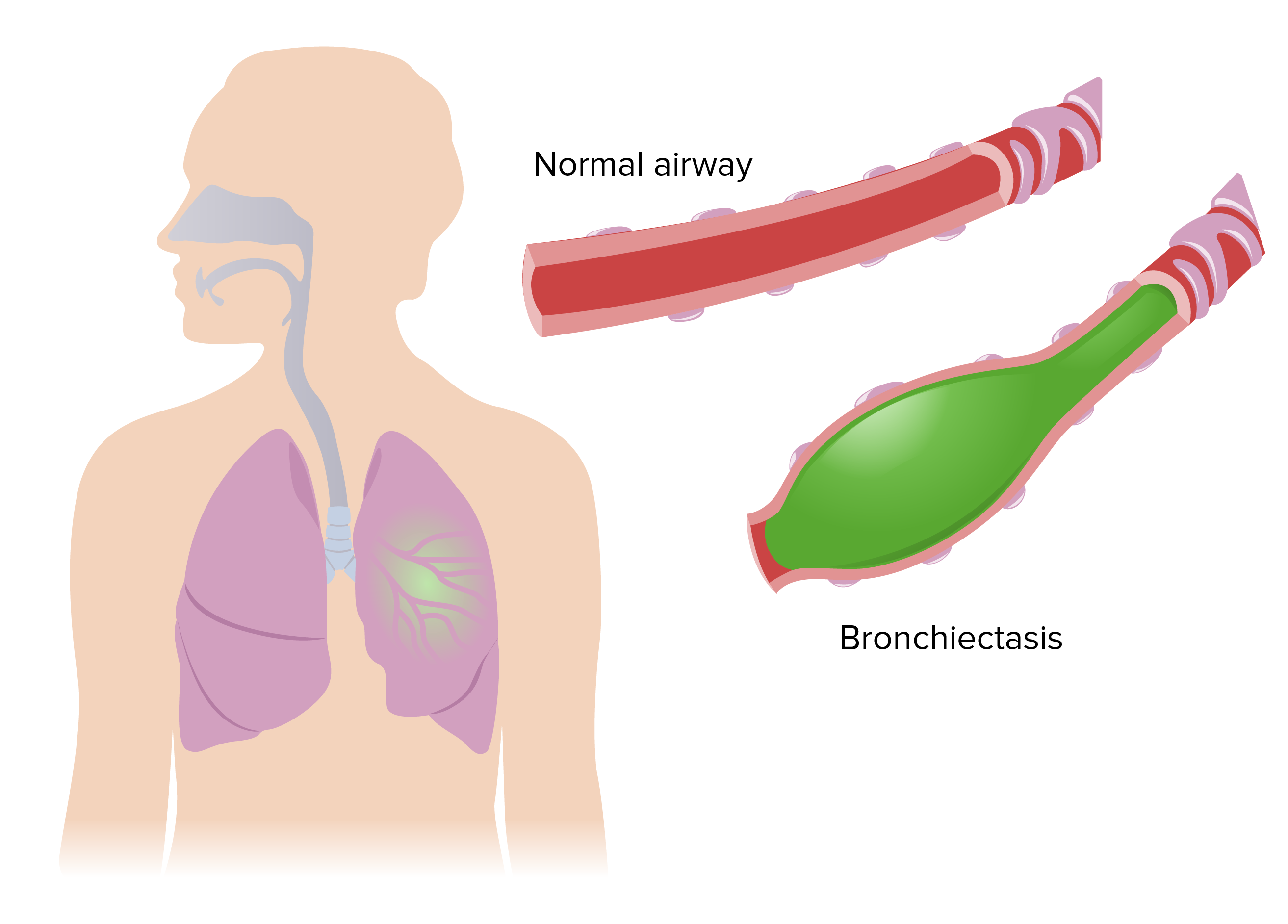
By Ricardo G. on 02. June 2020 for Bronchiectasis: Overview and Causes
Excellent teacher , he is a very good teacher , explains all with perfect detail , i liked the image of a cross section of the bronchi and the mucociliary elevator
Good lecture
By Ivan K. on 30. April 2020 for Asthma: Lower Airways Obstruction
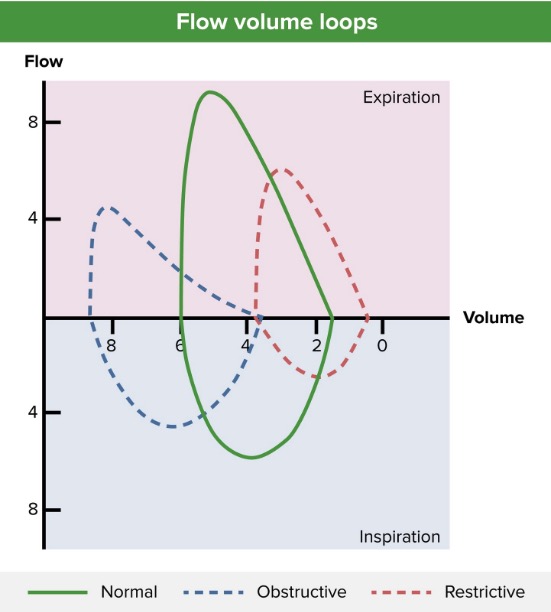
Good lecture. Well explained and with good illustration without much of text info in slides
I like it!
By Carolina M. on 20. April 2020 for Airway Diseases
I understand many things with this video class, the difference between asma and COPD, the diagnosis and treatment, etc. It was nice.
Well Explained
By Sudheer H. on 10. January 2020 for Asthma: Lower Airways Obstruction
Very well Explained, Very good faculty. All the required stuff in the lecture.
Great lecture as an introduction to asthma.
By Judas V. on 10. December 2019 for Asthma: Lower Airways Obstruction
I really liked this lecture a lot and I wanted to say it because of a rude coment that I saw on the comment section
Well explained
By Andrea Karolina G. on 03. April 2019 for Asthma: Treatment
I Like the way he explained this subjet, to the point, short and sweet
Got bored easily
By Nasser A. on 16. May 2018 for Airway Diseases
The way of teaching is boring and I felt I got lost with him
THE BEST REVIEW COURSE in the planet
By carlos m. on 31. March 2018 for Airway Diseases
Dr Brown delivers the content in a very effective way, easy to remember and also the information is up to date in accordance with recent Guidelines...
Excellent
By KHALED F. on 22. March 2018 for Airway Diseases
The lectures are very useful and valuable. The explanation is very clear.
VERY GOOD
By Khalid A. on 26. February 2018 for Chronic Obstructive Pulmonary Disease (COPD): Treatment
VERY GOOD LECTURE AD SDFG DFRD SDESSA SEDSF DFD SDFFG
interesting
By Temitope A. on 02. December 2017 for Airway Diseases
The lectures are interesting. I enjoyed listening to them. They are comprehensive and straightforward.
A GREAT REFRESHING COURSE
By javid d. on 31. December 2016 for Airway Diseases
GREETINGS; I chose this rating 'coz there is always scope for perfection .What i liked about this course was JEREMY Sir's style of teaching n his core understanding of the subject n the way he presented it.