Playlist
Show Playlist
Hide Playlist
Acute Ischemic Stroke (AIS): Diagnosis
-
Emergency Medicine Bord Acute Ischemic Stroke.pdf
-
Download Lecture Overview
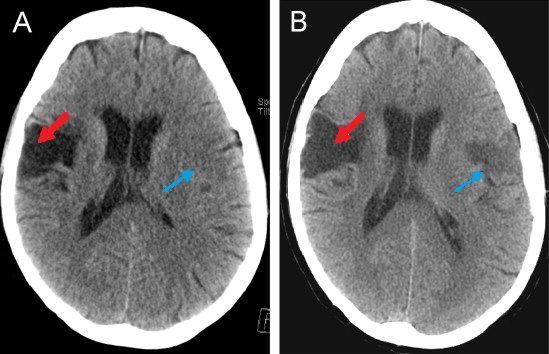
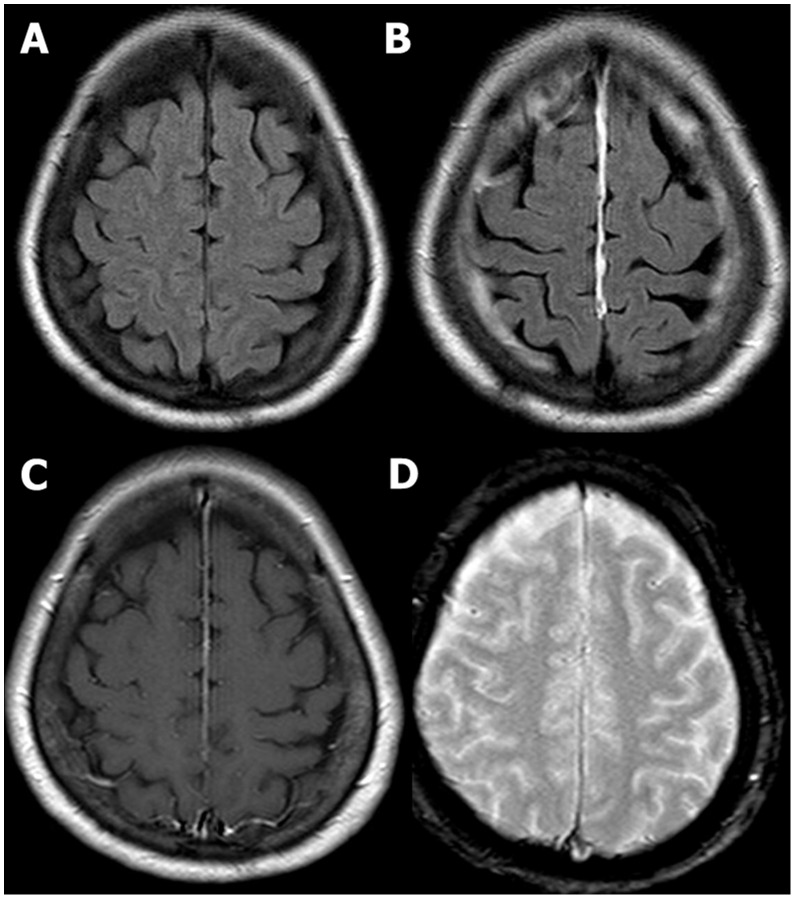
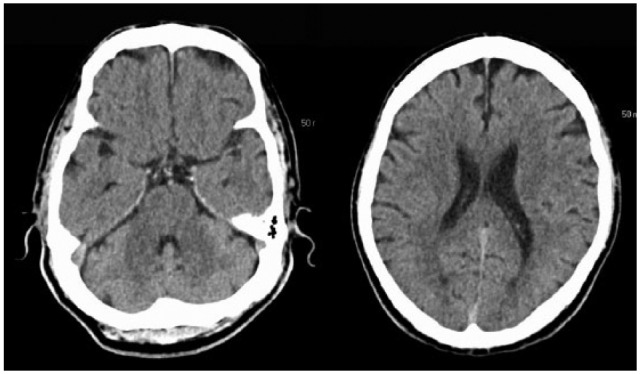
00:01 When patients present with these stroke symptoms, with weakness or sensory deficits, we wanna make sure that we’re keeping our differential still broad because we don’t wanna miss other things that could potentially be going on. 00:12 The first and critical thing to think about would be hypoglycemia. 00:16 Hypoglycemia or low blood sugar can present with a wide range of symptoms and definitely patients who are presenting with weakness, you wanna make sure you check a blood sugar. 00:27 Epidural or subdural hematoma are bleeding on the brain and you wanna make sure you’re thinking about that when you’re evaluating your patient. 00:35 Abscess or a brain mass can sometimes present with focal symptoms. 00:40 A migraine headache can sometimes also present with focal neurologic symptoms. 00:45 There’s something called Todd’s post-ictal paralysis. 00:49 What this basically is, is it’s a stroke mimic that can happen after a patient has a seizure. 00:54 So in that patient, it would be a patient that had a seizure and then when they come to the Emergency Department in their post-ictal state or their post-seizure state, they would have paralysis. 01:05 It actually can look very remarkably like a stroke. 01:08 Carotid or vertebral artery dissection is a tear in the intima or the wall of the vessel and that can look a lot like stroke symptoms. 01:18 And then cerebral venous sinus thrombosis which is a blood clot in the cerebral venous sinus. 01:24 The clinical pearl here, hypoglycemia is common. 01:27 I know we mention it a lot and we talk about it a lot, but it’s 100% reversible. 01:32 So always make sure you’re checking a blood sugar. 01:35 It’s something that actually believe it or not can be very easy to miss or to forget to do, so make sure you’re checking a finger stick glucose in all patients presenting with stroke symptoms. 01:45 When a patient arrives in the Emergency Department with stroke symptoms, one of the key first things we wanna do is get them a non-contrast head CT. 01:55 Again, our goal here is to figure out as quickly as possible whether or not a patient should get that clot busting medication if they’re having a stroke. 02:04 The non-contrast head CT is always a little confusing because that actually will not show you whether or not there’s an ischemic stroke there. 02:12 It will not show you whether or not there’s a blood clot there. 02:15 What it will show you is whether or not there’s any hemorrhagic stroke or bleeding in the brain and that’s important because if a patient has that, then they are most definitely not a candidate to get that clot busting medication. 02:27 The signs of infarction or stroke on the CT scan actually don’t occur until about six to 12 hours after the onset of symptoms. 02:36 So generally by that time, the patient is not a candidate anymore for the tPA medication. 02:41 So you really wanna make sure the first test they get generally right when they roll through the door is getting this non-contrast head CT. 02:50 The next thing that sometimes happens is an MRI, and you can get an MRI if you’re not totally certain whether or not a stroke has occurred. 02:58 Now, it used to be that MRI’s would take hours and hours and they would take a very long time for patients, but as time has progressed, MRI has become a lot more available in Emergency Departments for acute strokes or to help evaluate acute strokes. 03:11 And we get something called a hyperacute protocol. 03:14 The details of it we don’t necessarily need to go over here but basically what it can do is it can detect evidence of early stroke on that MRI and can indicate whether or not the patient would benefit from clot busting medication. 03:27 Now, MRI, like I said, this is one that can be done very quickly because we really know that we wanna limit the amount of time and workup of the patient. 03:36 Another important test to get is the EKG. 03:39 And the EKG is mainly looking for atrial fibrillation. 03:43 Atrial fibrillation is when the heart beats irregularly and the atria, the top portion of the heart fibrillate and what that means is that the blood sits in the atria, that portion of the heart for longer than it should be there. 03:56 And when the blood sits there for longer than it should be there, that patient – that blood has the tendency to form clots and when that blood forms a clot, that clot can then in turn go to the brain and cause a stroke. 04:08 So we’re looking mainly for arrhythmia when we get our EKG. 04:12 The last thing is blood tests. 04:14 Blood glucose, again, is on there because I really wanna make sure that that’s something that you remember to do. 04:20 Other important blood tests to get are coagulation testing. 04:24 So especially if your patient is on anticoagulation medication, you wanna go ahead and you wanna get that test done. 04:31 So when you’re taking your history from your patient, in addition to getting all of that other information, you also wanna try and ascertain whether or not your patient is on blood thinner or not on blood thinner, and then a CBC to help evaluate blood counts as well. 04:45 Electrolyte testing and other testing may be indicated but those are the tests that you wanna get immediately in the Emergency Department and have those sent stat so they get results in as quickly as possible.
About the Lecture
The lecture Acute Ischemic Stroke (AIS): Diagnosis by Sharon Bord, MD is from the course Neurologic and Psychiatric Emergencies.
Included Quiz Questions
Which among the following is LEAST frequently a differential diagnosis for acute ischemic stroke?
- Septic shock
- Hypoglycemia
- Brain mass
- Migraine
- Epidural hematoma
Which of the following is the preferred imaging study at most centers for the initial evaluation of probable ischemic stroke?
- Brain computed tomography scan without contrast
- Brain computed tomography scan with intravenous contrast
- Brain magnetic resonance imaging with gadolinium
- Serum level of fibrinolytic degradation products
- Carotid Doppler ultrasound
Which of the following heart conditions is most commonly seen in embolic stroke?
- Atrial fibrillation
- Anterior wall myocardial infarction
- Ventricular flutter
- Second degree atrioventricular block
- Electrical alternans
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
5 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |