Playlist
Show Playlist
Hide Playlist
Acute Inflammation: Stages – Inflammation and Wound Repair
-
Slides Inflamation Cellular Pathology.pdf
-
Download Lecture Overview
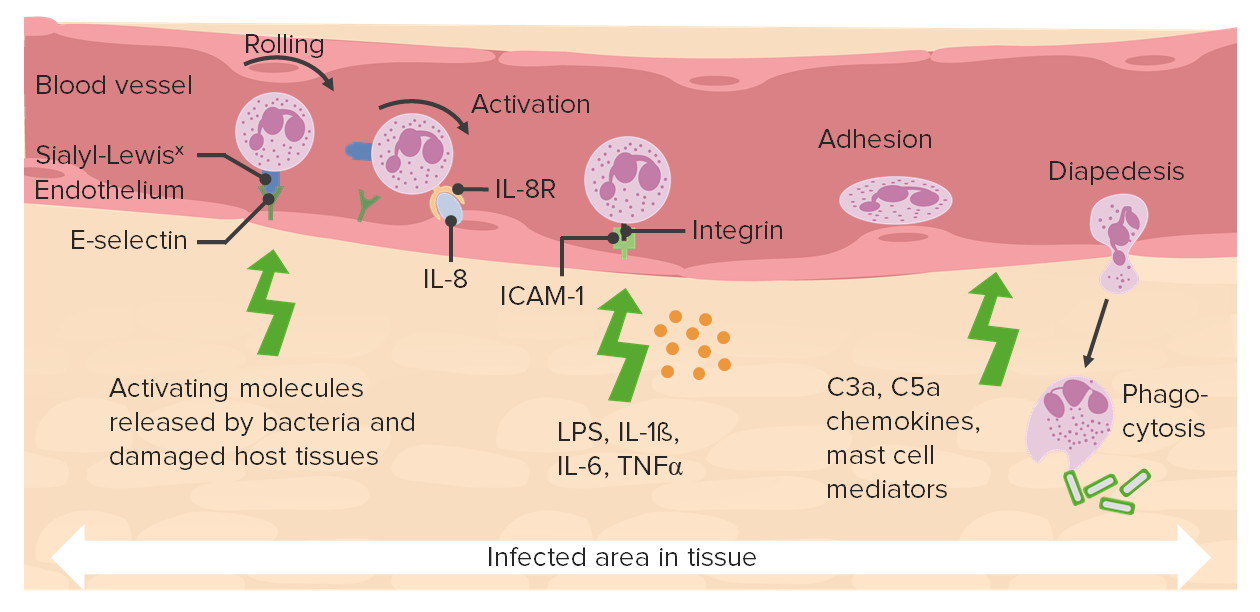
00:01 Acute inflammation, very transiently you are going to go into fight or flight mode. The sympathetic response kicks in. 00:10 And your blood vessels are vasoconstricting. This is not what you want for acute inflammation. This is not the state that you wish your blood vessels to be in so then you can facilitate the transmigration of neutrophil from the blood vessel into the interstitium. So therefore what is it. What component or chemical or peptide is then responsible for overcoming the initial vasoconstriction. Obviously histamine. Neurogenic is the response, vasoconstriction. Very transient. And shortly thereafter, you will have vasodilation of the arteriole and the major component that results in such a vasodilation we talked about is histamine. Responsible for your swelling, the tumor. The redness, the rubor. The calor, the heat. 00:58 Remember also that bradykinin then causes your pain and that's called your dolor. And your fifth and final cardinal sign with inflammation. Imagine if you've sprained your ankle. If you sprained your ankle then at some point you expect there to be inflammation don't you. And if you have inflammation taking place do you think that you might feel pain. Or even sensations have been lost. That's because of inflammation there might be compression of your nerves, or compromise of proper impulses, neuronal impulses, resulting in functio laesa, loss of function. What then happens when you have vasodilation? Well, I want you to go anatomically in the blood veessel from the capillary out towards your venule. Are you there? This will be the major site of how you can get your neutrophil permeable through your blood vessel into the interstitium. This of course also histamine will be responsible for. What then happens here? Well once you have the vasodilation taking place initially, that type of fluid which is escaping into the interstitium is your transudate, initial. This is due to increased hydrostatic pressure. 02:14 This is only fluid initially, can you picture it. Fluid is now escaping from your blood vessel into the interstitium due to vasodilation and as a result of a increased hydrostatic pressure. What then happens? Well eventually neutrophil gets out and let's say that this neutrophil is targetting a bacteria in the interstitium. If the neutrophil is targetting a bacteria in the interstitium and it undergoes the process of phagocytosis. You are going to now fill up the interstitium with lots of protein. 02:44 So therefore as a rule of thumb inflammation ultimately the type of edemea that you are going to find will be exudate, protein rich. Initially it will be protein poor. Blood flow movement into the interstitial space along with you have tons of protein. 03:01 The neutrophil is then going to marginate. What does that mean to you? It means that now, instead of being in a normal laminar flow, you are then going to get out into the margin. And when it does, well this is a good thing. Now what ends up happening is loss of axial stream due to rouleaux formation perhaps. By that we mean, often times with acute inflammation due to the margination that is taking place, remember please. Your focus here with acute inflammation is going to be the neutrophil, right. 03:32 You move from the circulating pool into the marginating pool. Obviously all blood flow has been affected in acute inflammation. 03:39 So therefore you can expect loss of axial stream and maybe perhaps a development of stacking of the RBC's Let's get into the specifics of acute inflammation. Things that you want to know. So here is my neutrophil that you are trying to get out into the interstitium. The first thing that has to happen as I told you is that the neutrophil has to come out into the margin. 04:03 This is margination. Initially, when the neutrophil comes out in the margin, it does not stop immediately. So therefore, this loose affinity of the neutrophil to the endothelium is an interaction called rolling. The major cytokines that you want to know that mediates rolling will be IL-1 and TNF. Pay attention to that. What is it that has a loose affinity. 04:34 Can you picture the endothelium for me. And the neutrophil with the leucocyte. Loose affinity. Has loose affinity, it's going to roll. Because it's marginating, it's marginating. Think of a plane crashing. I know that it seems rather morbid but it helps. 04:51 A plane crashes but when it does it's going to slide. That's what the neutrophil is doing. It's sliding on the margin. Are we clear. 04:58 That's selectin. In Immunology remember those selectins that are on the endothelial cell. E-selectin, P-selectin. Good. 05:08 This will then bind on to what on your neutrophil? Good, sialyl Lewis X. Remember that. Sialyl Lewis X. 05:17 If you are not familiar with that or if you are not good with this right now, it might be good idea for you to skip over to Immunology and get a real good handling for acute inflammation at least and come back here to pathology with me. At some point, the plane is crashing, we talked about rolling, and eventually the plane stops. This is called adhesion. The neutrophil is now adherent to whom? Where are you? Where is the neutrophil? Adherent to the wall of your blood vessel. In the meantime tell me about the state of my blood vessel right now. Vasodilated due to histamine, right. So you have that rubor, calor, tumor so on and so forth. 05:57 What is responsible for actual adhesion? The mediators here would be, well C5a and LTB4. It's a complement and leukotriene B4. 06:08 We'll talk more about C5a/Leukotriene B4 won't we. Of course we will. We'll talk about this as part of your chemotactic complex, chemotactic factors. Okay so, in the meantime, we have adhesion of the neutrophil to the endothelial cell. What are these called as a family? Integrins, integrins. You must memorise CD11, CD18. You must. Why? Once again, in Immunology, we talked about a particular disease called leucocyte adhesion deficiency. Leucocyte adhesion deficiency. There are two major types, there are more. 06:47 But there is one and two that you definitely want to pay attention to. And of those two, you pay attention to one. Focus more on one. 06:55 So, leucocyte adhesion deficiency type 1. This was an adhesion deficiency that took place congenitally that particular mutation there is a loss of CD11, CD18. Memorise that. First LAD type 1, there is a loss of CD11, CD18. So therefore you don't have adhesion. How is your young child going to present? There is going to be ulcers maybe around the mucosa or mucosa around the genital region which don't heal. Just keep this in mind, that there might be delayed separation of the umbilical cord. 07:36 Okay. Delayed separation umbilical cord. All pointing you towards your LAD and especially CD11, CD18 deficiency, LAD type 1. 07:46 What do this bind to on the endothelial cell? These are then called your ICAM and VCAM. So we have your cellular adhesion molecules. 07:55 So we have a couple of mediators here as well. Group them all together interleukin-1/TNF will play a role. As will C5a/LTB4. 08:04 If that discussion of cortisone catecholamine was inhibition of activation of adhesion. Our next topic would be activation of adhesion. 08:13 So what have you done now. Do you understand the language becomes important. If it's activation of adhesion molecules that means that neutrophils are going to marginate or demarginate please? It will marginate. You're moving your circulating pool into the marginating pool. Examples; endotoxins, sepsis. You are going to decrease in neutrophils. Remember once again, when you do a CBC, what are you measuring? The circulating pool or the marginating pool? Good, the circulating pool. 08:49 So if you marginate, you've taken the neutrophil out of the circulating pool you've put it into the margin. 08:56 Because you've activated what? The adhesion molecules. That has to be clear. Because you've done that, laboratory wise it's going to show you neutropenia. And leucocyte adhesion deficiency is what you are paying attention to, specifically type 1. 09:15 And I have asked you to please memorise CD11, CD18 deficiency resulting in such a state and this newborn is then may or may have a history of delayed separation of the umbilical cord. And if the child becomes injured, and so there is an ulcer that may develop in the genital region or in the mucosal region that it has a hard time. The ulcer will not heal properly. Welcome to LAD type 1 and just to make sure that you are clear from Immuno that if it's leucocyte adhesion type 2nd, then it's a deficiency of sialyl Lewis X. But your focus should be upon LAD type 1. In this step of acute inflammation, we'll take a look at transmigration. 09:59 Let me set up the picture first. We have a tubule here. This tubule is a blood vessel. Inside the blood vessel we have those blue cells that you are seing that line the blood vessel. Those are called endothelial cells. Inside the blood vessel you see that gray cell. 10:14 Our focus should be on the specific leucocyte called your neutrophil obviously with segmentation. If it's transmigration remember that the blood vessels now undergone vasodilation due to the help of your histamine. You can then expect there to be rubor, redness; and your tumor your swelling; and calor, we talked about heat emission. The first step is when the neutrophil is then loosely binding to the endothelial side and this step is called rolling. And the specific markers or the binding is through your selectins. 10:49 E-selectin, P-selectin, L-selectin and sialyl Lewis X will be playing roles with selectin sometimes referred to as being your addressins. Eventually, the neutrophil slow down, it will stop. You have your adhesion. And with adhesion we're referring to our integrin. And I told you that you needed to know about what may then happen when there is a mutation of CD11, CD18 resulting in LAD type 1. Next, our step is this. You'll notice please that the neutrophil on the very end of the tube on the right is making it's way through the endothelial cell. You see that. It literally going to then shoot out what's called this feet diapedesis. It's shooting out this feet so that it can pull the neutrophil through your blood vessel. This is transmigration. 11:43 Once you get the neutrophil down into your interstitium what's going to happen next is the fact that neutrophil through chemotaxis is going to then approach your bacteria. Now at this point, is when we call this exudate and majority of inflammation and the time that it spends in the type of fluid meaning to say transudate or exudate, would be exudate. The chemotactic factors as you remember from Immuno would be C5a/LTB4. Remember, the neutrophils come out of interstitium, brave new world, Ah, I don't know where to go, help me. So you have your chemotactic factors. This is the GPS for the neutrophil. It tells the neutrophil where to go. Chemicals that help you with taxing. Okay. So now you approached the bacteria. You also have interleukin-8 and remember in microbiology you've talked about (inaudible) right. Meaning to say bacterial product which will attract the neutrophil towards it. That's crazy. It's almost like saying Here, come here, kill me. Right. Whatever. Our body uses it to our advantage. So what do you think the next step will be. You have chemotaxis, neutrophil come to the bacteria, now we're going to have phagocytosis.
About the Lecture
The lecture Acute Inflammation: Stages – Inflammation and Wound Repair by Carlo Raj, MD is from the course Cellular Pathology: Basic Principles with Carlo Raj.
Included Quiz Questions
What best describes the nature of the fluid associated with swelling of tissue in acute inflammation?
- Initially a transudate
- Cell-rich transudate
- Protein-poor exudate
- Protein-rich exudate
- Protein-poor transudate
What is the first step in neutrophils entering the interstitium? (mediated by IL1 and TNF)
- Rolling
- Adhesion
- Margination
- Transmigration
- Endocytosis
During the adhesion process, what activates the integrins on the neutrophils?
- C5a/LTB4
- ICAM/VCAM
- IL1/TNF
- CD18
- CD11
What are absent in a patient with leukocyte-adhesion deficiency syndrome I?
- CD11 and CD18
- C5a and LTB4
- IL1 and TNF
- ICAM and VCAM
- CD4 and CD8
What is associated with WBC margination in a patient with sepsis?
- Neutropenia
- Leukocytosis
- Neutrophil adhesion defect
- Thrombocytopenia
- Inhibition of neutrophil adhesion molecules
What is the function of chemotactic factors?
- Signaling to neutrophils for effective pathogen clearance
- Mediation of transmigration
- Transition from transudate to exudate
- Rolling and adhesion
- Destruction of bacterial proteins
Customer reviews
4,8 of 5 stars
| 5 Stars |
|
3 |
| 4 Stars |
|
1 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
Very clear and helpful to understand the physio. Dr. Raj's lecture also was great because he went step by step and explained the stages more like a story which makes it easier to remember.
there is a confusion between cds and sylial on neutrophiles, overall it was good
I thought it was just like my professor very concise, with powerful imagery.
Only been using this site a few days. However I am already impressed by your material. Perfect execution of rhetorical techniques. Especially placing things in context with vivid verbal imagery.