Playlist
Show Playlist
Hide Playlist
Inflammatory Bowel Disease (IBD): Treatment
-
Slides Small and large bowel.pdf
-
Download Lecture Overview
00:01 Management. 00:02 Talked about aminosalicylic acid; topical rectal, oral, IV corticosteroids; Amino modulators, azathioprine, 6 mercaptopurine; anti-TNF therapy, but you are always worried about reactivation TB; antibiotics? Levaquin, Flagyl; total parenteral nutrition, especially for Crohn´s but due to malnutrition; surgery, be very careful with Crohn´s, because of the delicate nature of the disease with Crohn´s that you might actually cause more harm than good. 00:34 The aminosalicylic acid, what is it? Local anti-inflammatory. 00:42 What it does is inhibition of the cox pathway. 00:46 More effective in colonic than ileal disease, can induce and maintain remission, usually used for ulcerative colitis. Why? Why? Ulcerative colitis only involves the colon, and so therefore, when you give an enema, or you give a rectal type of administration, understand that you are more effective in the colon that you would be in the ileum, therefore more effective with ulcerative colitis. 01:18 Side effects occur in 30%, sulfasalazine much more so than mesalamine. 01:27 Nausea, rash, hair loss, hemolysis, pancreatitis, hepatitis, aplastic anemia, are things that you want to keep in mind. Sulfasalazine. 01:37 Corticosteroids. Topical preparation, or preparation needed for more proximal extensive disease, especially if it is Crohn´s. IV preparation for the severely ill, useful for induction but not for maintenance, the significance side effects of long terms we have talked about this quite a bit. 01:56 The fact that you might be lymphopenic, the fact that you might then cause a vast necrosis of the bone resulting in destruction and fractures. 02:05 Corticosteroids, of course, over long period of time, a common cause of iatrogenic type of Cushing´s. 02:15 The Anti-TNF Therapy. 02:16 Monoclonal antibody, have you heard of infliximab? Speaking -umab, you also have adalimumab and certolizumab. 02:24 The three preparations available in the US. 02:28 Do not forget about adalimumab. 02:30 Better response in Crohn's disease, use for both induction and maintenance here for anti-TNF. 02:37 Effective for the fistulizing disease. 02:43 Remember, in Crohn's disease much more fistula-like because a transmural involvement. 02:47 There's increase risk, of course, any type that you use anti-TNF therapy. 02:52 Remember what TNF, tumor necrosis factor. 02:55 It's responsible for inducing and maintaining your granuloma that's importantly required to contain the TB organism. 03:04 And if there's a granuloma has been lost due to anti-TNF therapy, outcomes the bacteria, reactivation TB. 03:15 Azathioprine or 6 Mercaptopurine. Immunosuppressive medication. 03:20 Here for maintenance of remission and steroid sparing effect. 03:26 A long half-life, side effects, pancreatitis, bone marrow suppression and hepatitis. 03:31 Also, keep in mind, that you also worried about administering 6MP, an allopurinol, because remember xanthine oxidase is required for proper metabolism of 6MP. 03:42 Azathioprine would be the precursor for 6MP. 03:47 Antibiotics, cipro and metronidazole commonly used for Crohn's. 03:53 Not useful in ulcerative colitis, antibiotics. 03:56 Long term use of metronidazole, associated with peripheral neuropathy, do not forget that and also with metronidazole do not forget about disulfiram-like effects. 04:07 TPN and bowel rest. 04:10 Not useful in UC but in Crohn's. 04:14 Diversion of fecal stream, colostomy and perianal diseases especially. 04:19 And total parenteral nutrition use pre-operatively for Crohn's to improve nutritional status. 04:25 Surgery, colectomy is curative for ulcerative colitis and indicated for intractable disease, megacolon, colon cancer and the site of anastomosis most likely recurrence to Crohn's disease. 04:44 Frequent re-operations among patients with Crohn's can lead to short gut syndrome. 04:52 Remember, the more that ended up taking out of your intestine, the more that you have or less that you have left. 05:01 Therefore, may manifest as mal-absorption, short gut syndrome.
About the Lecture
The lecture Inflammatory Bowel Disease (IBD): Treatment by Carlo Raj, MD is from the course Small and Large Intestine Diseases: Basic Principles with Carlo Raj.
Included Quiz Questions
Which of the following is NOT a side effect of sulfasalazine used in the treatment of inflammatory bowel disease?
- Peptic ulcer disease
- Hemolysis
- Hair loss
- Aplastic anemia
- Pancreatitis
A patient is diagnosed with ulcerative colitis, for which he began treatment. His hemoglobin level dropped, and a CBC report showed pancytopenia. When consulted by a hematologist, the patient forgot the name of the drug he had begun to receive. Which drug had the patient received?
- Sulfasalazine
- Doxycycline
- Prednisone
- Metronidazole
- Albendazole
Which complication is effectively treated by the use of anti-TNF therapy for Crohn's disease?
- Fistulas
- Oral ulcers
- Primary sclerosing cholangitis
- Arthritis
- Uveitis
A patient was diagnosed with Crohn's disease, for which anti-TNF therapy was planned. During the treatment, which tests must be performed periodically to prevent a frequent complication of the treatment?
- Mantoux test and chest X-ray
- Urine analysis and ultrasound scan of abdomen
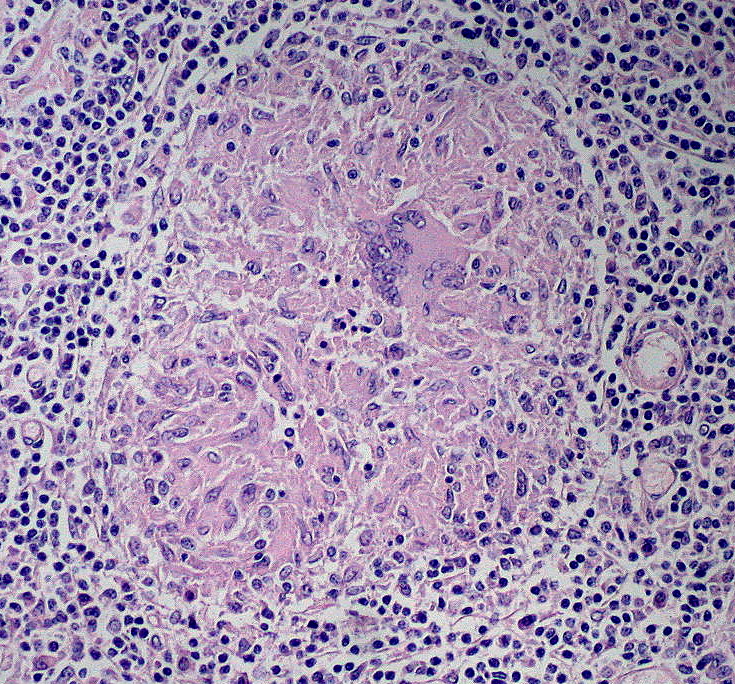
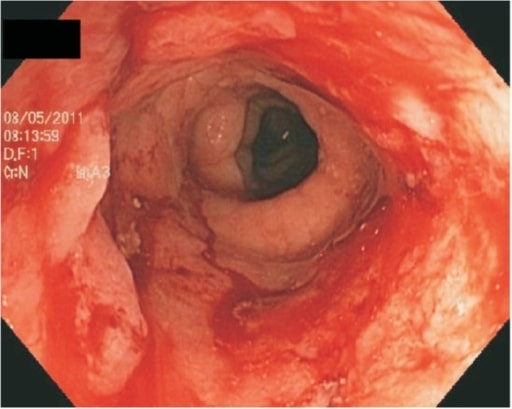
- Colonoscopy and biopsy
- Bence-Jones protein and skull X-ray
- PT/APTT and INR
Which test is helpful to identify side effects of azathioprine when used for the treatment of inflammatory bowel disease?
- Pancreatic amylase
- Beta HCG levels
- Prostate-specific antigen levels
- Urinary stercobilin levels
- TSH levels
Customer reviews
5,0 of 5 stars
| 5 Stars |
|
1 |
| 4 Stars |
|
0 |
| 3 Stars |
|
0 |
| 2 Stars |
|
0 |
| 1 Star |
|
0 |
These lectures are very informative, detailed. I learned a lot from the lectures.