Benign Benign Fibroadenoma or nonacute scrotal masses are represented by hydroceles, varicoceles, and spermatoceles. Key components to evaluation are physical exam and scrotal ultrasound. Hydroceles represent extra fluid in the tunica vaginalis Tunica vaginalis Testicles: Anatomy, leading to a swollen scrotum Scrotum A cutaneous pouch of skin containing the testicles and spermatic cords. Testicles: Anatomy. Varicoceles have a dilatation of the pampiniform venous plexus, giving the “bag of worms” appearance on exam. Spermatoceles present as an epididymal cyst, commonly arising from the head of the epididymis Epididymis The convoluted cordlike structure attached to the posterior of the testis. Epididymis consists of the head (caput), the body (corpus), and the tail (cauda). A network of ducts leaving the testis joins into a common epididymal tubule proper which provides the transport, storage, and maturation of spermatozoa. Testicles: Anatomy. Hydroceles, varicoceles, and spermatoceles are usually asymptomatic and do not require treatment unless they are causing pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways or other complications.
Last updated: Nov 14, 2022
Varicocele is the dilatation of the pampiniform venous plexus, which is connected to the internal spermatic or gonadal vein.
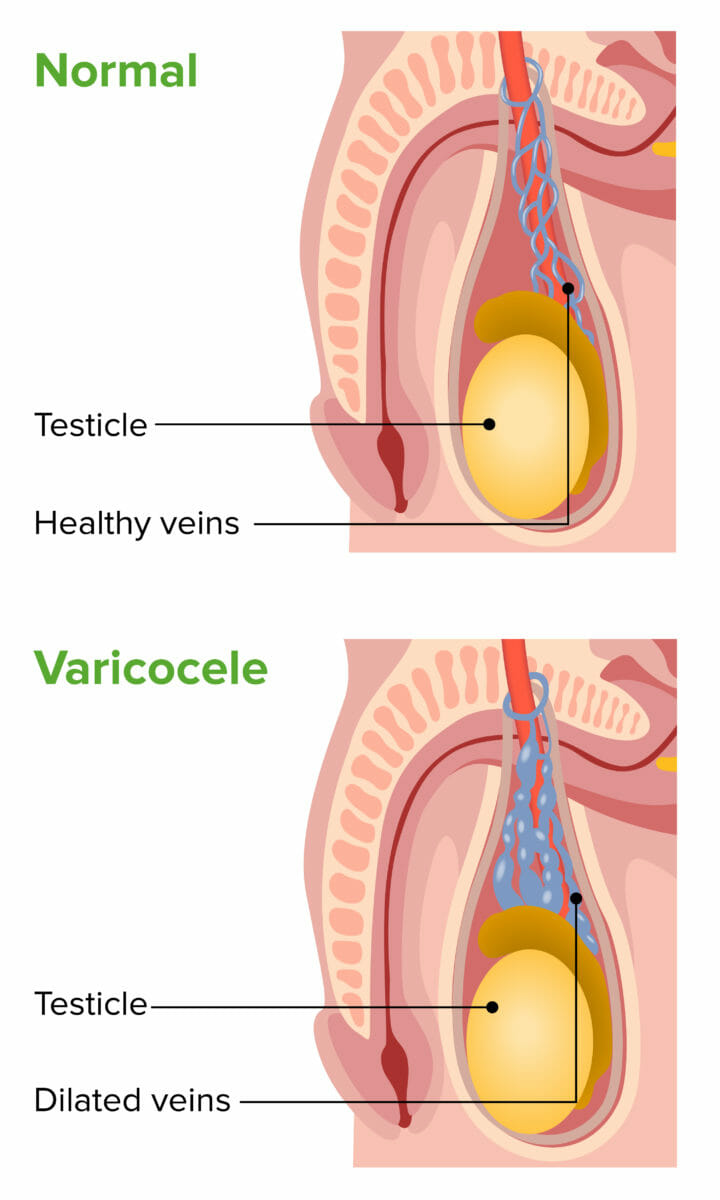
Varicocele: image showing left-sided dilated pampiniform venous plexus in the scrotum
Image by Lecturio.Examination:
Imaging (scrotal ultrasound):
Treatment approach:
Clinical considerations:
Hydrocele is a collection of peritoneal fluid in the tunica vaginalis Tunica vaginalis Testicles: Anatomy surrounding the testes Testes Gonadal Hormones. If bloody, the condition is referred to as hematocele.
Multifactorial, consisting of anatomic and fluid factors:

Hydrocele: enlarged scrotal mass filled with fluid
Image: “Hydrocele” by Dan Mischianu et al. License: CC BY 2.0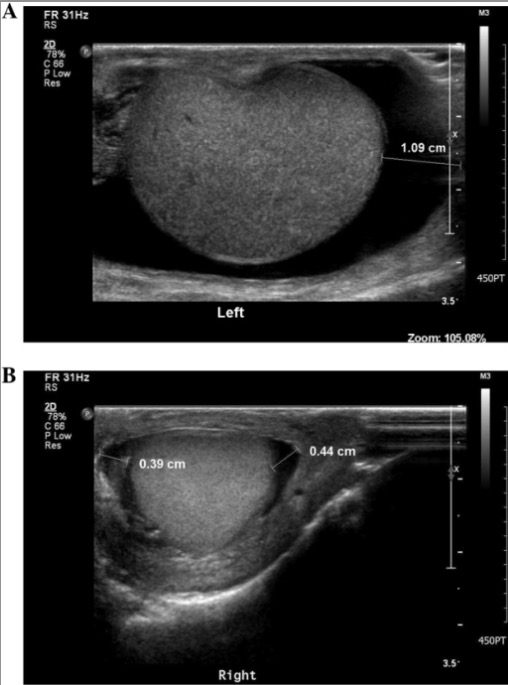
Transverse view of scrotal ultrasound showing hydrocele:
A: large left hydrocele as noted by the dark border delineating fluid surrounding the normal testicle in grey color
B: a smaller amount of fluid as a small hydrocele of the right testicle
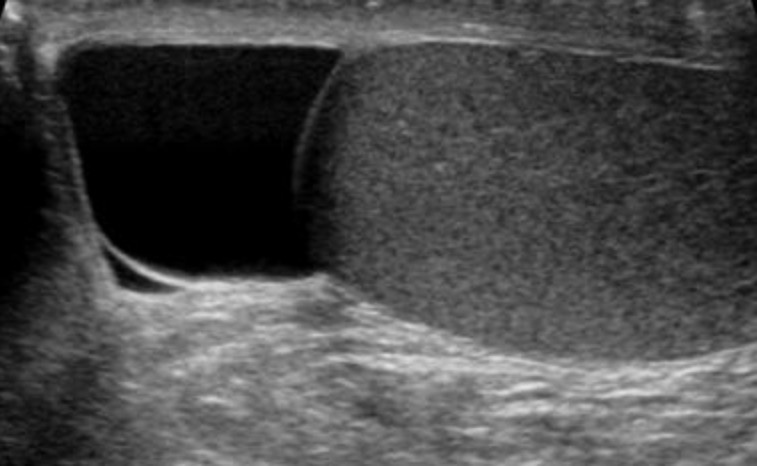
Transverse view of a scrotal ultrasound: Testicle is grey structure to the right and spermatocele is fluid-filled sac on the left (darker).
Image: “Spermatocele” by Iwak. License: Public DomainScrotal swelling Swelling Inflammation or mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast has the following differential diagnoses: