Sudden infant death syndrome (SIDS) describes the sudden death of an otherwise healthy infant (< 1 year of age) with no identifiable cause. Sudden infant death syndrome is the leading cause of death in children between 1 and 12 months of age in the United States. Sudden infant death syndrome is a diagnosis of exclusion and can only be confirmed after other causes of death have been ruled out with a thorough medical history and autopsy. Providing parents with preventative education is key to reducing the risk of SIDS. Preventative measures include having infants sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep supine, on firm surfaces, with no clutter in their crib.
Last updated: Sep 29, 2022
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of a child in infancy (< 1 year of age) with no identifiable cause after examination, clinical case review, and autopsy.
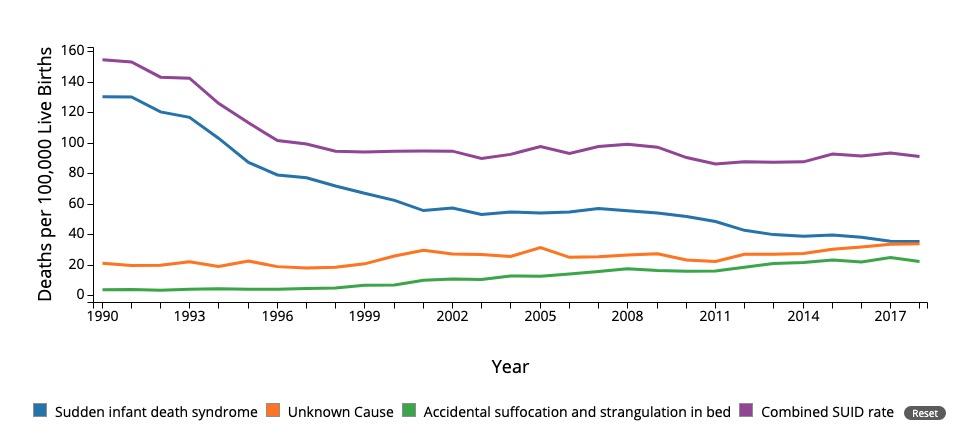
Mortality due to sudden infant death syndrome (SIDS) and other causes. Notice the decrease since 1994 due to public interventions including the “back to sleep” campaign.
SUID: Sudden unexpected infact death
The most likely cause of SIDS involves a multifactorial genesis in particularly vulnerable babies, in which internal and external factors work together.
SIDS is a diagnosis of exclusion that can be assigned only after:
The primary focus of management is providing an accurate post-mortem diagnosis as well as emotional and psychological support to the parents. Parents and family members should also be:
Parental education is key to preventing SIDS. As noted above, many of the risk factors are modifiable and can be prevented. Parental education includes:
The following conditions are natural causes of death to be distinguished from SIDS: