Menopause is a physiologic process in women characterized by the permanent cessation of menstruation Menstruation The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle that occurs after the loss of ovarian activity. Menopause can only be diagnosed retrospectively, after 12 months without menstrual bleeding. During the menopausal transition, reproductive hormones Hormones Hormones are messenger molecules that are synthesized in one part of the body and move through the bloodstream to exert specific regulatory effects on another part of the body. Hormones play critical roles in coordinating cellular activities throughout the body in response to the constant changes in both the internal and external environments. Hormones: Overview and Types can fluctuate significantly, leading to symptoms that include hot flushes Hot Flushes Primary Ovarian Insufficiency, sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep and mood disturbances, and vaginal dryness. In postmenopausal woman, low estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy levels contribute to an increased risk for cardiovascular disease, osteoporosis Osteoporosis Osteoporosis refers to a decrease in bone mass and density leading to an increased number of fractures. There are 2 forms of osteoporosis: primary, which is commonly postmenopausal or senile; and secondary, which is a manifestation of immobilization, underlying medical disorders, or long-term use of certain medications. Osteoporosis, and sexual dysfunction Sexual dysfunction Physiological disturbances in normal sexual performance in either the male or the female. Sexual Physiology due to vulvovaginal atrophy Atrophy Decrease in the size of a cell, tissue, organ, or multiple organs, associated with a variety of pathological conditions such as abnormal cellular changes, ischemia, malnutrition, or hormonal changes. Cellular Adaptation. For some women, symptoms negatively affect their quality Quality Activities and programs intended to assure or improve the quality of care in either a defined medical setting or a program. The concept includes the assessment or evaluation of the quality of care; identification of problems or shortcomings in the delivery of care; designing activities to overcome these deficiencies; and follow-up monitoring to ensure effectiveness of corrective steps. Quality Measurement and Improvement of life and treatment is warranted. Management usually involves menopausal hormone therapy (MHT), but other treatment options also exist.
Last updated: Sep 29, 2022
Menopause is the permanent physiologic cessation of menses Menses The periodic shedding of the endometrium and associated menstrual bleeding in the menstrual cycle of humans and primates. Menstruation is due to the decline in circulating progesterone, and occurs at the late luteal phase when luteolysis of the corpus luteum takes place. Menstrual Cycle due to loss of ovarian activity determined retrospectively after 12 consecutive months of no menstrual bleeding and low estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy levels.
Menopause is characterized by a physiologic ↓ in oocytes Oocytes Female germ cells derived from oogonia and termed oocytes when they enter meiosis. The primary oocytes begin meiosis but are arrested at the diplotene state until ovulation at puberty to give rise to haploid secondary oocytes or ova (ovum). Ovaries: Anatomy due to progressive atresia Atresia Hypoplastic Left Heart Syndrome (HLHS), ultimately leading to a chronic hypoestrogenic state in postmenopause. During the menopause transition, hormone levels fluctuate significantly.
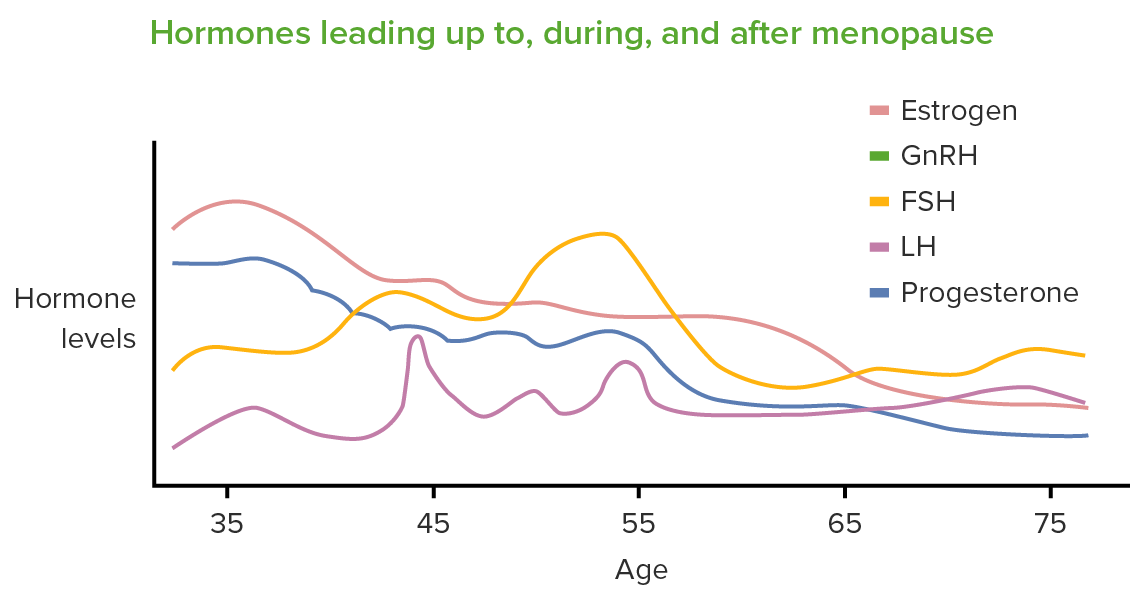
The primary hormonal changes seen in perimenopause/menopause are a decrease in estrogen and progesterone and an increase in follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
GnRH: gonadotropin-releasing hormone
Normal oocyte counts:
Effects of estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy:
Late reproductive years/early menopause transition:
Late menopause transition:
Primary estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy switches from estradiol Estradiol The 17-beta-isomer of estradiol, an aromatized C18 steroid with hydroxyl group at 3-beta- and 17-beta-position. Estradiol-17-beta is the most potent form of mammalian estrogenic steroids. Noncontraceptive Estrogen and Progestins (E2) to estrone Estrone An aromatized C18 steroid with a 3-hydroxyl group and a 17-ketone, a major mammalian estrogen. It is converted from androstenedione directly, or from testosterone via estradiol. In humans, it is produced primarily by the cyclic ovaries, placenta, and the adipose tissue of men and postmenopausal women. Noncontraceptive Estrogen and Progestins ( E1 E1 An aromatized C18 steroid with a 3-hydroxyl group and a 17-ketone, a major mammalian estrogen. It is converted from androstenedione directly, or from testosterone via estradiol. In humans, it is produced primarily by the cyclic ovaries, placenta, and the adipose tissue of men and postmenopausal women. Noncontraceptive Estrogen and Progestins):
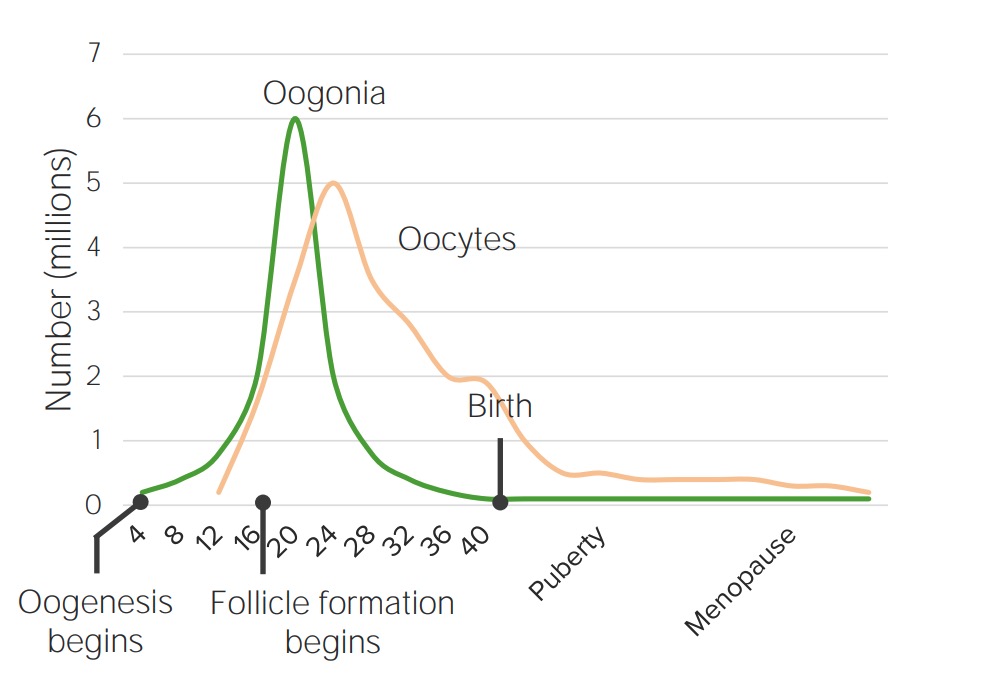
Oocyte counts over lifespan of a woman:
Oogenesis is mostly completed by birth and viable oocyte counts continue to decrease through a woman’s life.
| Hormone | Change | Explanation |
|---|---|---|
| Anti-Müllerian hormone ( AMH AMH A glycoprotein that causes regression of mullerian ducts. It is produced by sertoli cells of the testes. In the absence of this hormone, the mullerian ducts develop into structures of the female reproductive tract. In males, defects of this hormone result in persistent mullerian duct, a form of male pseudohermaphroditism. Primary Amenorrhea) | ↓ |
|
| Inhibin B | ↓ |
|
| LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle and FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle | ↑ | Inhibin B has an inhibitory effect on LH LH A major gonadotropin secreted by the adenohypophysis. Luteinizing hormone regulates steroid production by the interstitial cells of the testis and the ovary. The preovulatory luteinizing hormone surge in females induces ovulation, and subsequent luteinization of the follicle. Luteinizing hormone consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle and FSH FSH A major gonadotropin secreted by the adenohypophysis. Follicle-stimulating hormone stimulates gametogenesis and the supporting cells such as the ovarian granulosa cells, the testicular sertoli cells, and leydig cells. Fsh consists of two noncovalently linked subunits, alpha and beta. Within a species, the alpha subunit is common in the three pituitary glycoprotein hormones (TSH, LH, and FSH), but the beta subunit is unique and confers its biological specificity. Menstrual Cycle, so during menopause their levels increase. |
| Testosterone Testosterone A potent androgenic steroid and major product secreted by the leydig cells of the testis. Its production is stimulated by luteinizing hormone from the pituitary gland. In turn, testosterone exerts feedback control of the pituitary LH and FSH secretion. Depending on the tissues, testosterone can be further converted to dihydrotestosterone or estradiol. Androgens and Antiandrogens | ↓ |
|
The clinical symptoms of perimenopause are caused by fluctuating hormone levels in the menopause transition period. The presentation of postmenopause results from the low estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy levels that ensue after cessation of ovarian function, which persist for the remainder of a woman’s life.
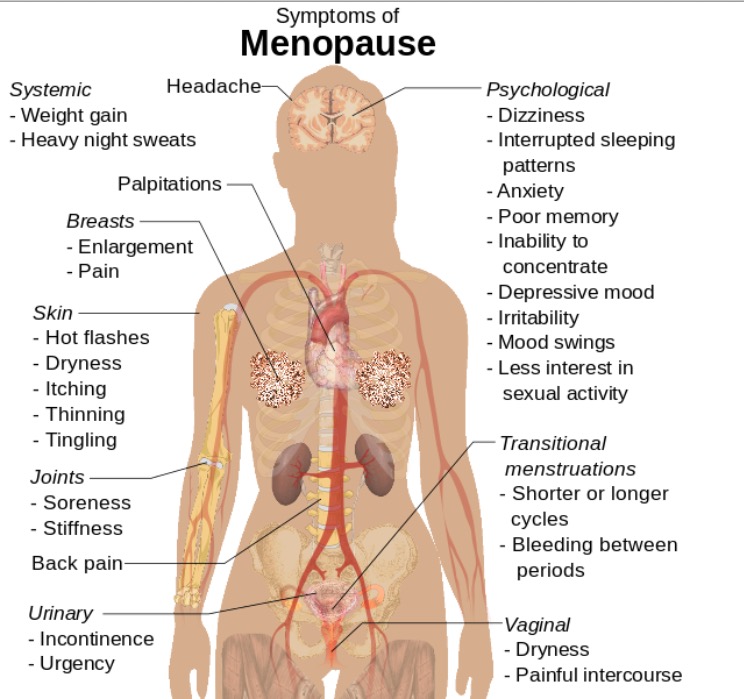
Symptoms of menopause that can also be seen in primary ovarian insufficiency
Image: “Symptoms of menopause” by Mikael Häggström. License: CC0These symptoms are a result of long-term estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy deficiency:
HAVOCS:
A majority of women in perimenopause and postmenopause do not require treatment. The primary goals of management are relief of bothersome symptoms and ensuring health through appropriate screening Screening Preoperative Care.
Estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy therapy (ET):
Progestins Progestins Compounds that interact with progesterone receptors in target tissues to bring about the effects similar to those of progesterone. Primary actions of progestins, including natural and synthetic steroids, are on the uterus and the mammary gland in preparation for and in maintenance of pregnancy. Hormonal Contraceptives:
Candidates for therapy:
Contraindications Contraindications A condition or factor associated with a recipient that makes the use of a drug, procedure, or physical agent improper or inadvisable. Contraindications may be absolute (life threatening) or relative (higher risk of complications in which benefits may outweigh risks). Noninvasive Ventilation to MHT include history of:
General principles:
Risks and benefits beyond symptom relief:
| Test | Frequency |
|---|---|
| Cervical cytology Cervical cytology A procedure in which ectocervical and endocervical cells are collected to evaluate the transformation zone (area at risk for cervical cancer). Cervical Cancer Screening | Up to age 65/every 3 years |
| Diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus testing | At age 45/every 3 years |
| Colonoscopy Colonoscopy Endoscopic examination, therapy or surgery of the luminal surface of the colon. Colorectal Cancer Screening | At age 50 (45 if at high risk)/every 10 years |
| Mammography Mammography Radiographic examination of the breast. Breast Cancer Screening | At age 40/annually |
| Bone Bone Bone is a compact type of hardened connective tissue composed of bone cells, membranes, an extracellular mineralized matrix, and central bone marrow. The 2 primary types of bone are compact and spongy. Bones: Structure and Types mineral density | At age 65/every 2 years if risk factors are present |