Nonalcoholic fatty liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease is a spectrum of liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy pathology that arises due to accumulation of triglycerides Triglycerides Fatty Acids and Lipids in hepatocytes Hepatocytes The main structural component of the liver. They are specialized epithelial cells that are organized into interconnected plates called lobules. Liver: Anatomy. Risk factors include diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, insulin resistance Insulin resistance Diminished effectiveness of insulin in lowering blood sugar levels: requiring the use of 200 units or more of insulin per day to prevent hyperglycemia or ketosis. Diabetes Mellitus, obesity Obesity Obesity is a condition associated with excess body weight, specifically with the deposition of excessive adipose tissue. Obesity is considered a global epidemic. Major influences come from the western diet and sedentary lifestyles, but the exact mechanisms likely include a mixture of genetic and environmental factors. Obesity, and hypertension Hypertension Hypertension, or high blood pressure, is a common disease that manifests as elevated systemic arterial pressures. Hypertension is most often asymptomatic and is found incidentally as part of a routine physical examination or during triage for an unrelated medical encounter. Hypertension, among others. Nonalcoholic fatty liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease ranges from fatty liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy or hepatic steatosis Hepatic Steatosis Imaging of the Liver and Biliary Tract but can lead to nonalcoholic steatohepatitis Steatohepatitis Drug-Induced Liver Injury (NASH), which features fatty deposits and inflammation Inflammation Inflammation is a complex set of responses to infection and injury involving leukocytes as the principal cellular mediators in the body's defense against pathogenic organisms. Inflammation is also seen as a response to tissue injury in the process of wound healing. The 5 cardinal signs of inflammation are pain, heat, redness, swelling, and loss of function. Inflammation. Progressive liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy injury and fibrosis Fibrosis Any pathological condition where fibrous connective tissue invades any organ, usually as a consequence of inflammation or other injury. Bronchiolitis Obliterans irreversibly develop into cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis and, possibly, primary liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy cancer. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship are usually asymptomatic but may present with hepatomegaly and right upper quadrant Right upper quadrant Anterior Abdominal Wall: Anatomy discomfort. Although liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma is the diagnostic gold standard, the diagnosis can also be established by clinical history, imaging, and laboratory tests. The mainstay of management is lifestyle modifications ( weight loss Weight loss Decrease in existing body weight. Bariatric Surgery and exercise) with control of associated comorbidities Comorbidities The presence of co-existing or additional diseases with reference to an initial diagnosis or with reference to the index condition that is the subject of study. Comorbidity may affect the ability of affected individuals to function and also their survival; it may be used as a prognostic indicator for length of hospital stay, cost factors, and outcome or survival. St. Louis Encephalitis Virus.
Last updated: Jan 18, 2024
Fatty liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy has alcoholic Alcoholic Persons who have a history of physical or psychological dependence on ethanol. Mallory-Weiss Syndrome (Mallory-Weiss Tear) or nonalcoholic subtypes.
Nonalcoholic fatty liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease (NAFLD):
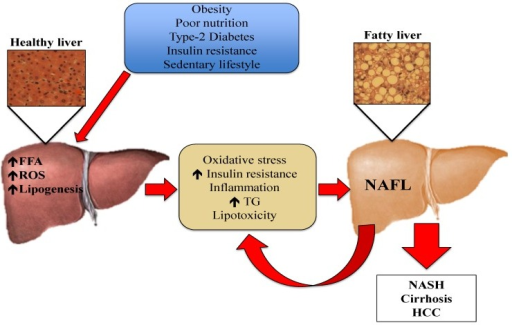
Pathogenesis of NAFLD: Risk factors such as obesity, poor nutrition, type 2 diabetes, insulin resistance, and sedentary lifestyle cause efflux of FFAs from the adipose tissue to the liver. The increased FFAs in hepatic tissue stimulate triglyceride (TG) synthesis and accumulation. This excess of lipids induces an immune response, causing the production of cytokines, reactive oxygen species (ROS), and worsening insulin resistance. Oxidative stress causes lipid peroxidation and tissue damage, amplifying the inflammatory response and leading to the progression of NAFLD.
HCC: hepatocellular carcinoma
NAFL: non-alcoholic fatty liver
NASH: non-alcoholic steatohepatitis
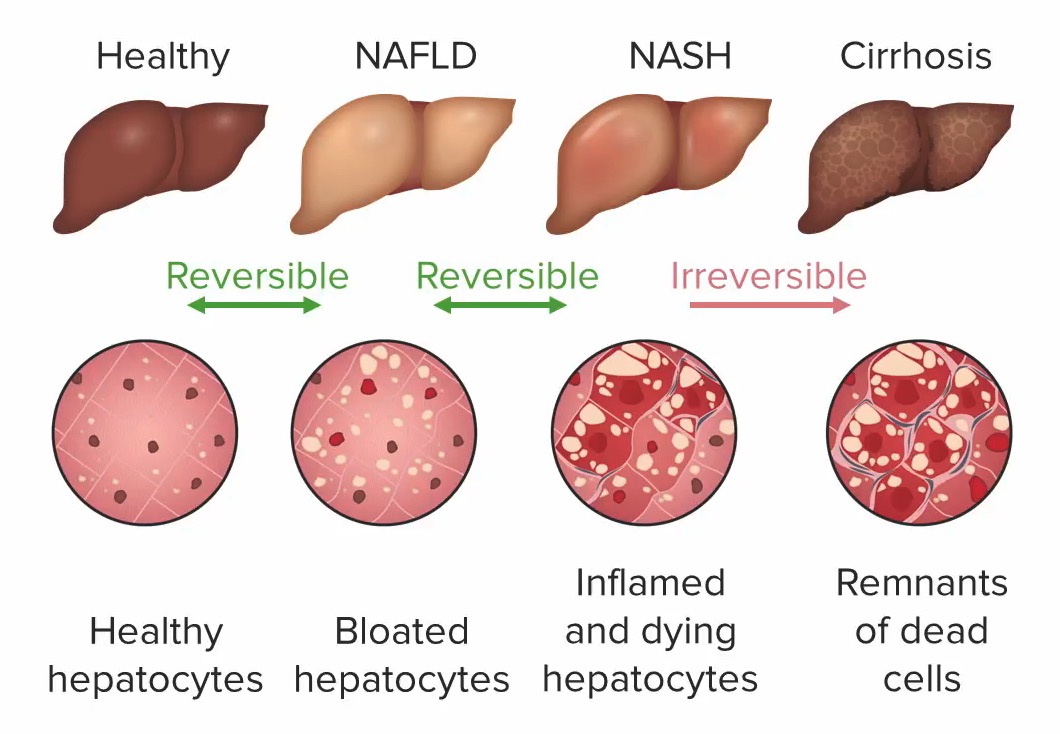
If progression is not reversed, NAFL leads to NASH. With further liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy damage, cirrhosis Cirrhosis Cirrhosis is a late stage of hepatic parenchymal necrosis and scarring (fibrosis) most commonly due to hepatitis C infection and alcoholic liver disease. Patients may present with jaundice, ascites, and hepatosplenomegaly. Cirrhosis can also cause complications such as hepatic encephalopathy, portal hypertension, portal vein thrombosis, and hepatorenal syndrome. Cirrhosis and liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy carcinoma (both irreversible) become potential outcomes:
Progression of liver disease due to steatosis:
1: Healthy hepatocytes: no liver damage
2: Bloated hepatocytes with steatosis (distended by fat droplets), no inflammation: NAFL/steatosis (still reversible)
3: Inflamed and dying hepatocytes, with possible fibrosis: nonalcoholic steatohepatitis (still reversible)
4: Dead cells: cirrhosis (irreversible liver damage)
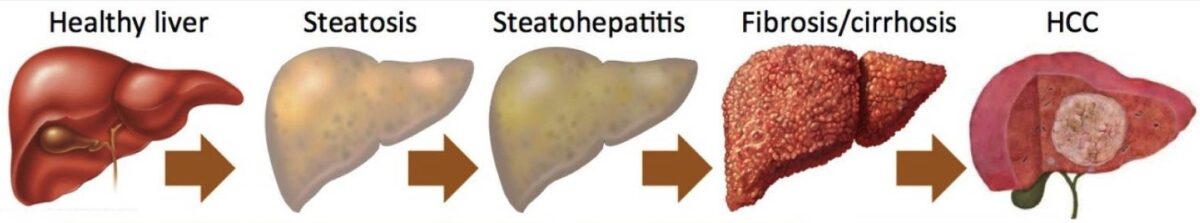
Progression of liver disease: steatosis to HCC
Image: “Nonalcoholic fatty liver disease” by Department of Medicine, VA Boston Healthcare System and Brigham and Women’s Hospital, Harvard Medical School, 150 S. Huntington Ave., Room 6A-46, Boston, MA 02130, USA. License: CC BY 4.0, edited by Lecturio.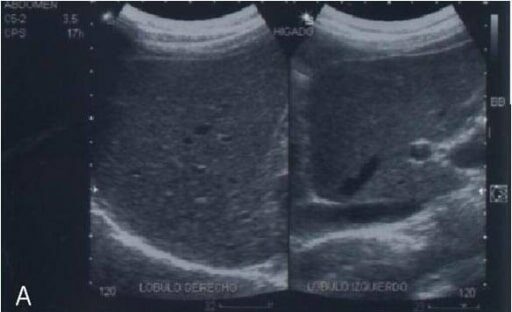
Abdominal ultrasonography of a patient with NAFD showing increased increased hepatic parenchyma echotexture due to fat infiltration (“brilliant liver”)
Image: “Abdominal ultrasonography of a patient with non-alcoholic fatty liver disease” by Department of Biochemistry, School of Medicine, National Autonomous University of Mexico (UNAM), Mexico, 04510, Mexico. License: CC BY 2.0, edited by Lecturio.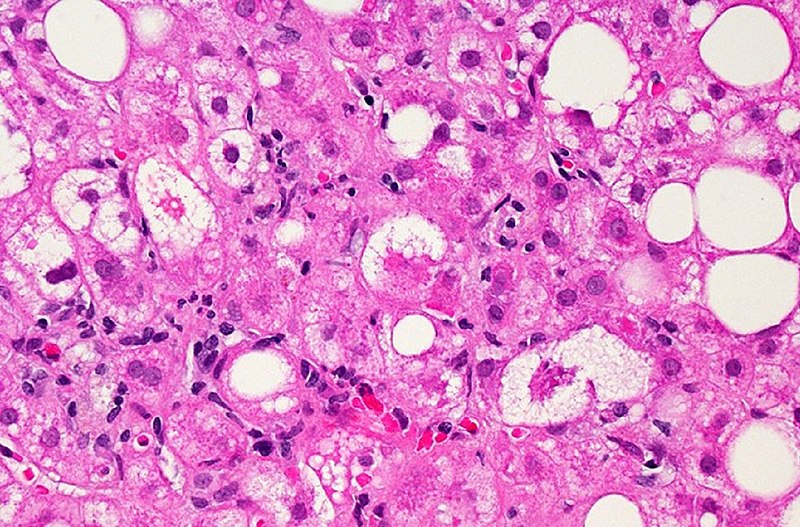
Microscopic image of liver tissue affected by NAFLD: The large and small white spots are excess fat droplets filling liver cells (hepatocytes).
Image: “Liver Tissue with NAFLD” by Dr. David Kleiner, National Cancer Institute/NIH. License: Public Domain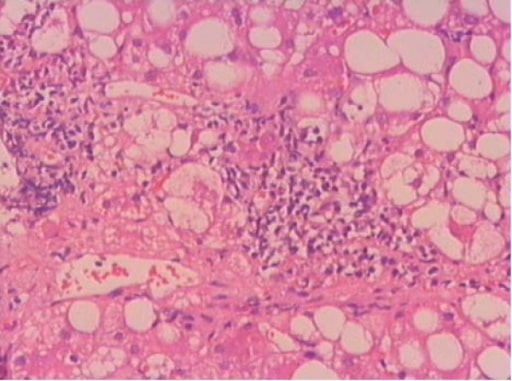
Portal inflammation is a diagnostic finding in NASH. Histopathologic section was obtained from a patient with steatohepatitis.
Image: “F1” by Gastroenterology Department, Ege University Faculty of Medicine, Izmir, Turkey. License: CC BY 2.0