Hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome is a reversible condition in which elevated ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance levels cause impaired brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification function in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with advanced liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease. Hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome can be precipitated by conditions that affect the normal absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption, metabolism, or clearance of ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance, including dehydration Dehydration The condition that results from excessive loss of water from a living organism. Volume Depletion and Dehydration, renal failure Renal failure Conditions in which the kidneys perform below the normal level in the ability to remove wastes, concentrate urine, and maintain electrolyte balance; blood pressure; and calcium metabolism. Renal insufficiency can be classified by the degree of kidney damage (as measured by the level of proteinuria) and reduction in glomerular filtration rate. Crush Syndrome, infections Infections Invasion of the host organism by microorganisms or their toxins or by parasites that can cause pathological conditions or diseases. Chronic Granulomatous Disease, and gastrointestinal bleeding Gastrointestinal bleeding Gastrointestinal bleeding (GIB) is a symptom of multiple diseases within the gastrointestinal (GI) tract. Gastrointestinal bleeding is designated as upper or lower based on the etiology's location to the ligament of Treitz. Depending on the location of the bleeding, the patient may present with hematemesis (vomiting blood), melena (black, tarry stool), or hematochezia (fresh blood in stools). Gastrointestinal Bleeding. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship present with a progression of symptoms, from minimal confusion and asterixis to stupor and coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma. Diagnosis is clinical and requires the exclusion of alternative diagnoses. Management involves addressing the causative factor and decreasing the systemic absorption Absorption Absorption involves the uptake of nutrient molecules and their transfer from the lumen of the GI tract across the enterocytes and into the interstitial space, where they can be taken up in the venous or lymphatic circulation. Digestion and Absorption of ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance with lactulose Lactulose A synthetic disaccharide used in the treatment of constipation and hepatic encephalopathy. It has also been used in the diagnosis of gastrointestinal disorders. Laxatives or rifaximin.
Last updated: Jan 17, 2024
Hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome is seen in patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship with severe liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease or liver failure Liver failure Severe inability of the liver to perform its normal metabolic functions, as evidenced by severe jaundice and abnormal serum levels of ammonia; bilirubin; alkaline phosphatase; aspartate aminotransferase; lactate dehydrogenases; and albumin/globulin ratio. Autoimmune Hepatitis, and can be exacerbated by:
Precipitating factors for hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome can be remembered by the mnemonic “HEPATICS”:
Normal physiology:
Liver Liver The liver is the largest gland in the human body. The liver is found in the superior right quadrant of the abdomen and weighs approximately 1.5 kilograms. Its main functions are detoxification, metabolism, nutrient storage (e.g., iron and vitamins), synthesis of coagulation factors, formation of bile, filtration, and storage of blood. Liver: Anatomy disease allows disruption of normal ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance regulation through:
Impaired brain Brain The part of central nervous system that is contained within the skull (cranium). Arising from the neural tube, the embryonic brain is comprised of three major parts including prosencephalon (the forebrain); mesencephalon (the midbrain); and rhombencephalon (the hindbrain). The developed brain consists of cerebrum; cerebellum; and other structures in the brain stem. Nervous System: Anatomy, Structure, and Classification function results from a buildup of ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance, where it:
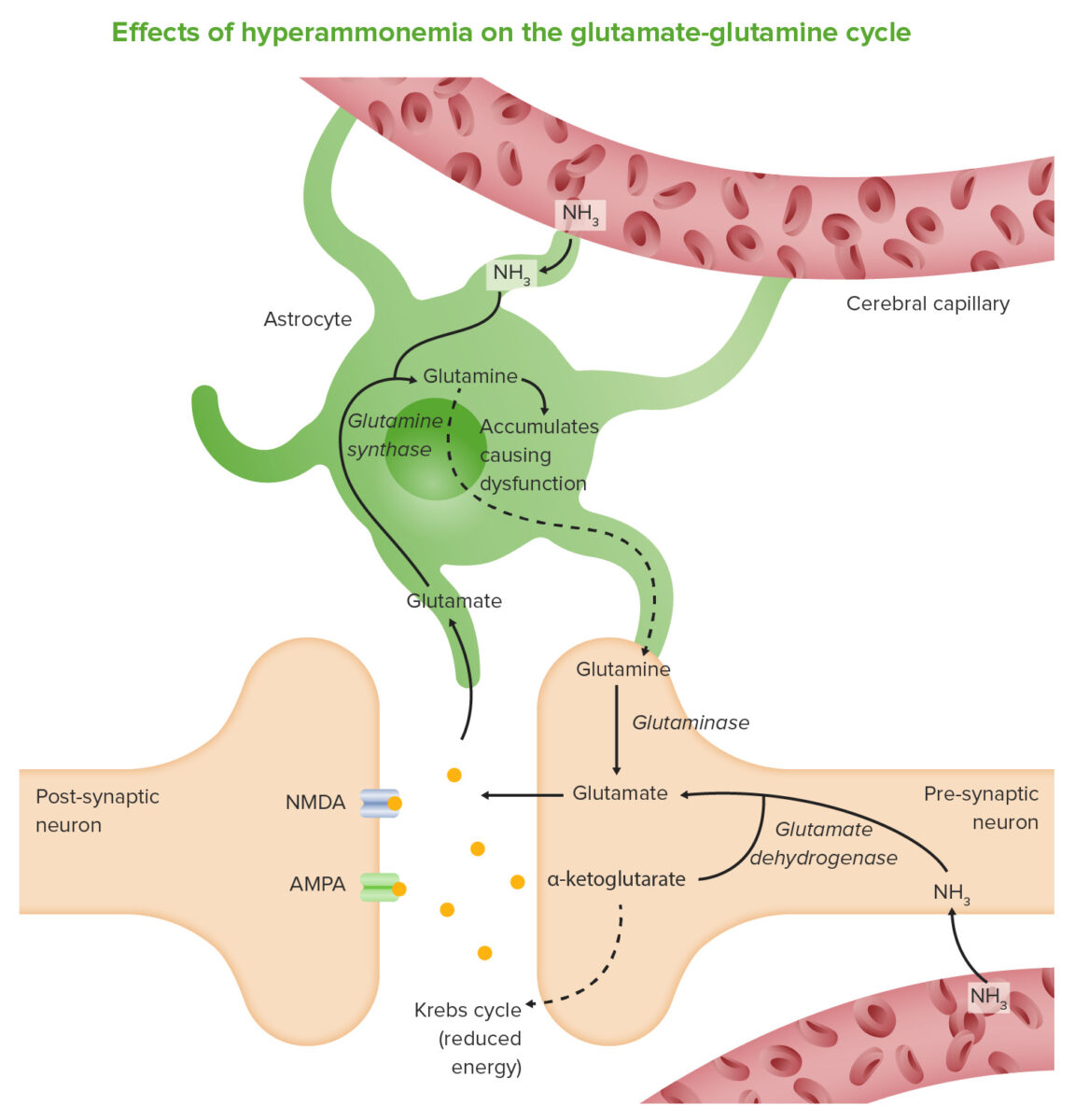
Ammonia (NH3) crosses the blood–brain barrier and is absorbed and metabolized by astrocytes. These cells use ammonia when synthesizing glutamine from glutamate. The increased levels of glutamine lead to a rise in osmotic pressure in the astrocytes, which become swollen and result in brain edema. Ammonia also increases activity of the inhibitory GABA system and reduces energy production.
Image by Lecturio.The West Haven criteria are used to grade the clinical severity.
| Grade | Consciousness | Intellect Intellect Psychiatric Assessment and behavior | Neurological findings |
|---|---|---|---|
| 0 | Normal | Normal | Normal |
| Minimal | Normal | Psychometric (psychomotor speed/executive function) or neurophysiologic tests are abnormal. | Psychometric (psychomotor speed/executive function) or neurophysiologic tests are abnormal. |
| 1 | Mild lack of awareness | Slowed intellect Intellect Psychiatric Assessment, apathy Apathy Lack of emotion or emotional expression; a disorder of motivation that persists over time. Wernicke Encephalopathy and Korsakoff Syndrome, restlessness, disordered sleep Sleep A readily reversible suspension of sensorimotor interaction with the environment, usually associated with recumbency and immobility. Physiology of Sleep | Mild asterixis, impaired computation |
| 2 | Lethargic | Moderate disorientation Disorientation St. Louis Encephalitis Virus, drowsiness, inappropriate behavior | Asterixis, slurred speech Slurred Speech Cerebellar Disorders |
| 3 | Somnolent but arousable | Disorientation Disorientation St. Louis Encephalitis Virus, incoherent speech | Asterixis, hyperreflexia, clonus Clonus Ehrlichiosis and Anaplasmosis, muscular rigidity Rigidity Continuous involuntary sustained muscle contraction which is often a manifestation of basal ganglia diseases. When an affected muscle is passively stretched, the degree of resistance remains constant regardless of the rate at which the muscle is stretched. This feature helps to distinguish rigidity from muscle spasticity. Megacolon |
| 4 | Coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma | Coma Coma Coma is defined as a deep state of unarousable unresponsiveness, characterized by a score of 3 points on the GCS. A comatose state can be caused by a multitude of conditions, making the precise epidemiology and prognosis of coma difficult to determine. Coma | Decerebrate or decorticate posturing Decorticate Posturing Increased Intracranial Pressure (ICP), asterixis is typically absent |
Hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome is a clinical diagnosis, and other conditions must be excluded.
Tip: Spontaneous bacterial peritonitis Spontaneous Bacterial Peritonitis Ascites should be ruled out in all patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship presenting with hepatic encephalopathy Encephalopathy Hyper-IgM Syndrome and ascites Ascites Ascites is the pathologic accumulation of fluid within the peritoneal cavity that occurs due to an osmotic and/or hydrostatic pressure imbalance secondary to portal hypertension (cirrhosis, heart failure) or non-portal hypertension (hypoalbuminemia, malignancy, infection). Ascites.
Management focuses on identifying and treating precipitating factors, and lowering the serum ammonia Ammonia A colorless alkaline gas. It is formed in the body during decomposition of organic materials during a large number of metabolically important reactions. Note that the aqueous form of ammonia is referred to as ammonium hydroxide. Acid-Base Balance concentration.