Variables represent information about something that can change. The design of the measurement scales Scales Dry or greasy masses of keratin that represent thickened stratum corneum. Secondary Skin Lesions, or of the methods for obtaining information, will determine the data gathered and the characteristics of that data. As a result, a variable can be qualitative or quantitative, and may be further classified into subgroups. Every possible way to express the value of a variable, or the range of the variable, is called a domain.
Last updated: Aug 8, 2022
A variable is a placeholder for a value that may be represented in a qualitative or quantitative manner. A function is a relationship Relationship A connection, association, or involvement between 2 or more parties. Clinician–Patient Relationship between multiple variables.
2 major classes of variables:
Within epidemiology:
In epidemiology, a variable is understood as a set of attributes.
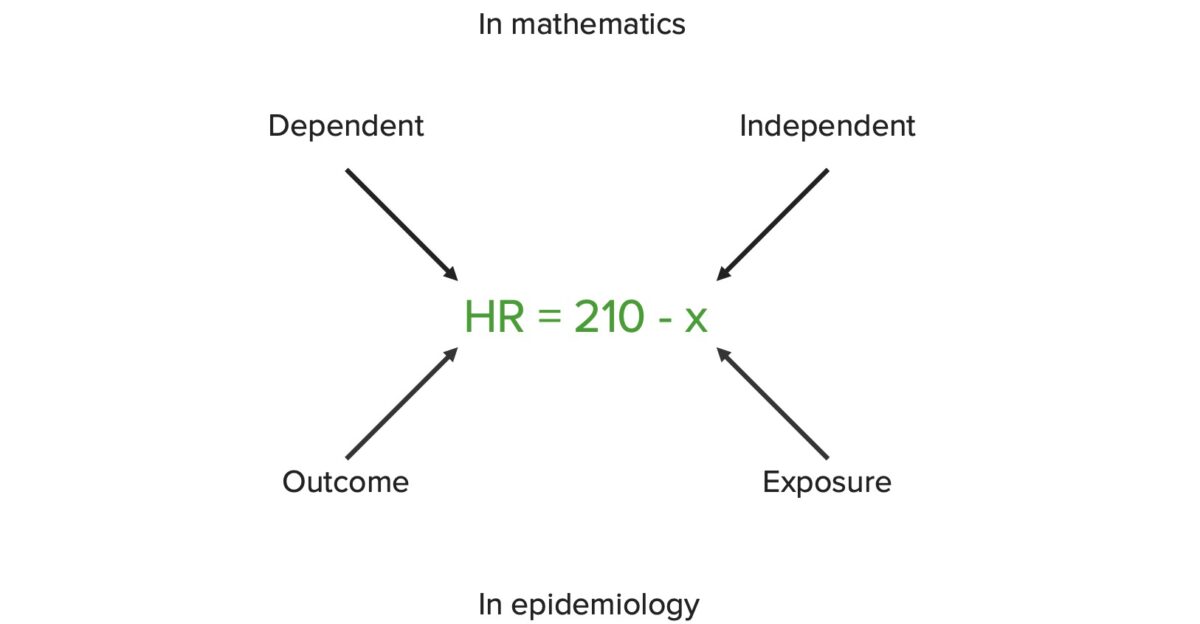
The distinct interpretations of the independent and dependent variables in mathematics and epidemiology:
This example illustrates a function commonly utilized to estimate the target exercise heart rate (HR) for a patient based on age. The patient’s age (x) can be changed, and is thus the independent variable (or exposure). HR represents the patient’s target exercise heart rate, and is calculated based on the independent variable. Because of this, HR considered the dependent variable (or outcome).
Nominal:
Ordinal or ranked:
Continuous:
Discrete: