Insulin is a peptide hormone that is produced by the beta cells of the pancreas Pancreas The pancreas lies mostly posterior to the stomach and extends across the posterior abdominal wall from the duodenum on the right to the spleen on the left. This organ has both exocrine and endocrine tissue. Pancreas: Anatomy. Insulin plays a role in metabolic functions such as glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance uptake, glycolysis Glycolysis Glycolysis is a central metabolic pathway responsible for the breakdown of glucose and plays a vital role in generating free energy for the cell and metabolites for further oxidative degradation. Glucose primarily becomes available in the blood as a result of glycogen breakdown or from its synthesis from noncarbohydrate precursors (gluconeogenesis) and is imported into cells by specific transport proteins. Glycolysis, glycogenesis Glycogenesis Glycogen Metabolism, lipogenesis Lipogenesis De novo fat synthesis in the body. This includes the synthetic processes of fatty acids and subsequent triglycerides in the liver and the adipose tissue. Lipogenesis is regulated by numerous factors, including nutritional, hormonal, and genetic elements. Nonalcoholic Fatty Liver Disease, and protein synthesis Synthesis Polymerase Chain Reaction (PCR). Exogenous insulin may be needed for individuals with diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus mellitus, in whom there is a deficiency in endogenous insulin or increased insulin resistance Insulin resistance Diminished effectiveness of insulin in lowering blood sugar levels: requiring the use of 200 units or more of insulin per day to prevent hyperglycemia or ketosis. Diabetes Mellitus. There are several forms of insulin, and they differ in their time of onset, peak effect, and duration. Insulin can be classified as fast acting, short acting, intermediate acting, or long acting. A combination of classes can be used to maintain glucose Glucose A primary source of energy for living organisms. It is naturally occurring and is found in fruits and other parts of plants in its free state. It is used therapeutically in fluid and nutrient replacement. Lactose Intolerance control throughout the day. Common adverse effects include hypoglycemia Hypoglycemia Hypoglycemia is an emergency condition defined as a serum glucose level ≤ 70 mg/dL (≤ 3.9 mmol/L) in diabetic patients. In nondiabetic patients, there is no specific or defined limit for normal serum glucose levels, and hypoglycemia is defined mainly by its clinical features. Hypoglycemia, weight gain after initiation of an insulin regimen, and local injection site changes.
Last updated: Sep 1, 2022
Insulin types can be classified based on their pharmacokinetics Pharmacokinetics Pharmacokinetics is the science that analyzes how the human body interacts with a drug. Pharmacokinetics examines how the drug is absorbed, distributed, metabolized, and excreted by the body. Pharmacokinetics and Pharmacodynamics:
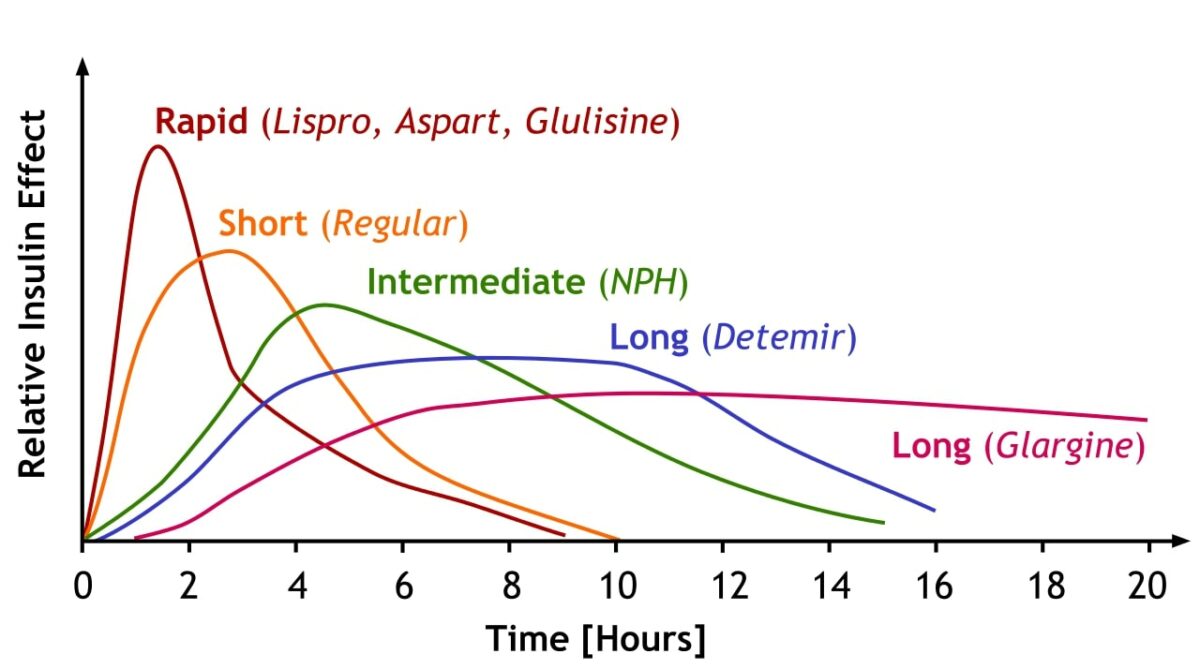
A comparison of the onset, peak effect, and duration of different insulin subtypes
Image: “Insulin is categorized by how fast it works in the body, how soon it peaks and then how long it lasts. Notice how rapid acting insulins have a rapid rise and fall while longer acting insulin builds more slowly to a stable baseline before declining.” by A. Peters, M. Komorniczak. License: CC BY 3.0Subcutaneous insulin:
IV insulin:
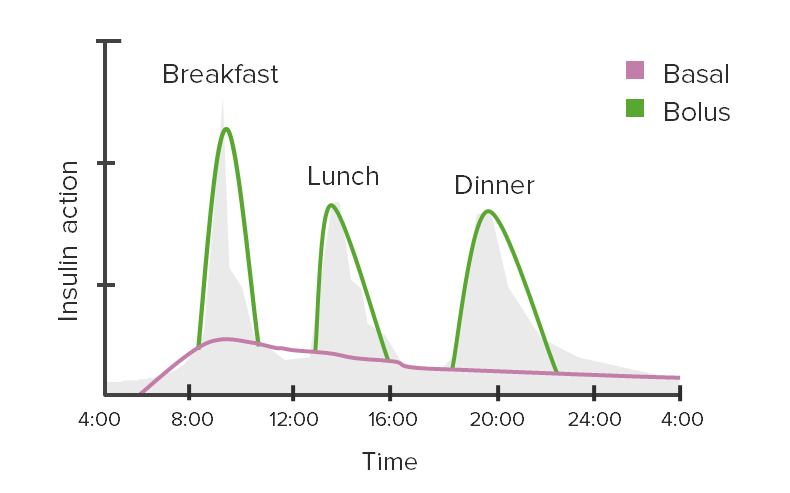
Glycemic excursions and insulin action:
This graph depicts the use of basal and bolus (meal-time) insulin to cover variations in blood glucose levels throughout the day.
Besides diabetes Diabetes Diabetes mellitus (DM) is a metabolic disease characterized by hyperglycemia and dysfunction of the regulation of glucose metabolism by insulin. Type 1 DM is diagnosed mostly in children and young adults as the result of autoimmune destruction of β cells in the pancreas and the resulting lack of insulin. Type 2 DM has a significant association with obesity and is characterized by insulin resistance. Diabetes Mellitus, IV insulin can be used in several other conditions (often in conjunction with dextrose Dextrose Intravenous Fluids to maintain euglycemia).
Dosing adjustments and close monitoring may be necessary for individuals with:
| Insulin effect | Type of Insulin | Classification | Onset of action | Peak of action | Duration of action |
|---|---|---|---|---|---|
| Fast acting | Lispro | Analog | 15–30 minutes | 1–3 hours | 4–6 hours |
| Aspart | |||||
| Glulisine | |||||
| Short acting | Regular | Human | 30 minutes | 1.5–3.5 hours | 8 hours |
| Intermediate acting | NPH NPH Normal pressure hydrocephalus (NPH) is a neurodegenerative disorder characterized by the triad of gait abnormalities, dementia, and urinary urgency or incontinence. Normal pressure hydrocephalus can be either idiopathic or secondary to intraventricular or subarachnoid hemorrhage. Normal Pressure Hydrocephalus | Human | 1–2 hours | 4–6 hours | > 12 hours |
| Long acting | Detemir | Analog | 1–2 hours | 3–9 hours | 14–24 hours |
| Glargine | 3–4 hours | No peak | Approximately 24 hours | ||
| Degludec | Approximately 1 hour | No peak | > 40 hours |