An aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms is the abnormal dilation of a segment of the aorta Aorta The main trunk of the systemic arteries. Mediastinum and Great Vessels: Anatomy. Abdominal aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms is the most common aortic aneurysm Aortic aneurysm An abnormal balloon- or sac-like dilatation in the wall of aorta. Thoracic Aortic Aneurysms, occurring frequently in the infrarenal area. Degenerative aortic disorders are the prevalent etiology, affecting patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship > 60 years of age. Most aneurysms are asymptomatic, but can cause compression Compression Blunt Chest Trauma of surrounding structures or rupture, which is a life-threatening emergency. Diagnosis is often made by ultrasound. As aneurysmal rupture Aneurysmal rupture The tearing or bursting of the weakened wall of the aneurysmal sac, usually heralded by sudden worsening pain. The great danger of a ruptured aneurysm is the large amount of blood spilling into the surrounding tissues and cavities, causing hemorrhagic shock. Thoracic Aortic Aneurysms carries a high mortality Mortality All deaths reported in a given population. Measures of Health Status rate, surveillance Surveillance Developmental Milestones and Normal Growth is recommended for asymptomatic cases to monitor aortic diameter. Elective surgery (the majority via endovascular aortic repair) is an effective way to reduce complications and aneurysm-related death. This surgery is performed based on aortic size, underlying condition, and associated symptoms.
Last updated: Nov 14, 2022
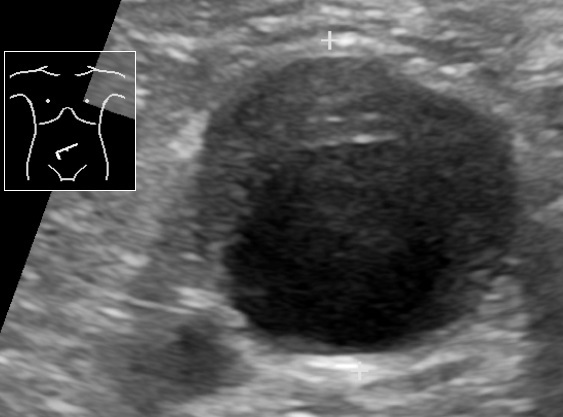
Ultrasound showing an abdominal aortic aneurysm with a mural thrombus
Image: “Ultrasonography of abdominal aortic aneurysm with mural thrombus” by Mikael Häggström, M.D.. License: Public Domain| AAA management of asymptomatic patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship (ultrasound) | AAA size |
|---|---|
| Rescreen after 10 years | ≥ 2.5 cm but < 3 cm |
| Imaging every 3 years | 3–3.9 cm |
| Imaging every 12 months | 4–4.9 cm |
| Imaging every 6 months | 5–5.4 cm |
| Consider elective repair | ≥ 5.5 cm Consider repair if ≥ 5 cm in women; expansion of < 0.5 cm/6 months or > 1 cm/1 year; associated femoral, iliac, popliteal aneurysm Popliteal aneurysm Extremity and Visceral Aneurysms, or PAD requiring revascularization Revascularization Thromboangiitis Obliterans (Buerger’s Disease) |
Indications for operative repair
Operative options