All-in-One Online Anesthesiology Course
Ace your anesthesiology exams with a customizable learning platform built by clinicians and medical educators.

Start the online anesthesiology class taught by Dr. Brian Warriner
Building on foundations of cardiovascular and respiratory physiology, this course will present the basics and types of anesthesia, go over the ins and outs of ICU environments, teach how to approach emergencies and go into the pathophysiology of pain. In addition, you will get practical tips from experienced educator Dr. Warriner, e.g. about how to handle difficult airways when intubating. Start studying now!
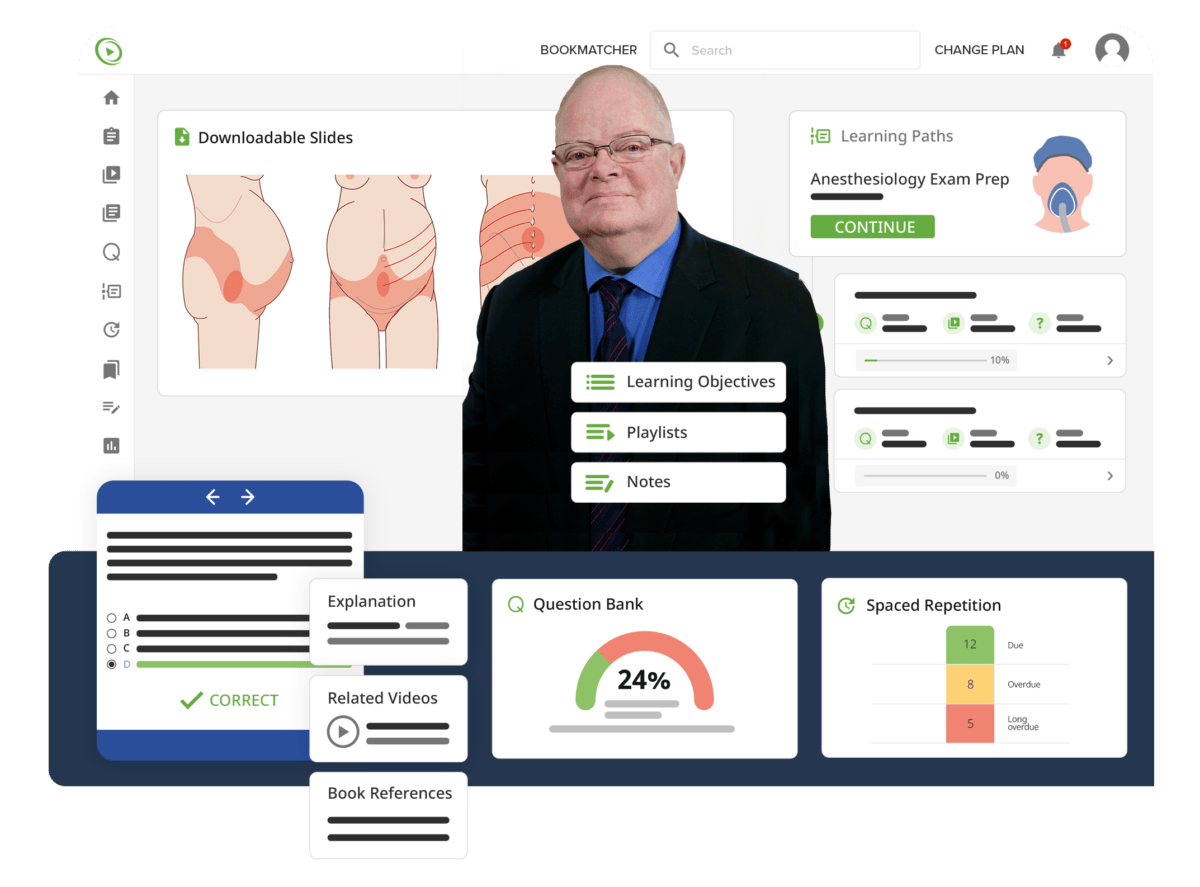
Diversify and Optimize Your Learning Strategy
Close your knowledge gap and solidify your understanding of anesthesiology
with a wide array of learning tools
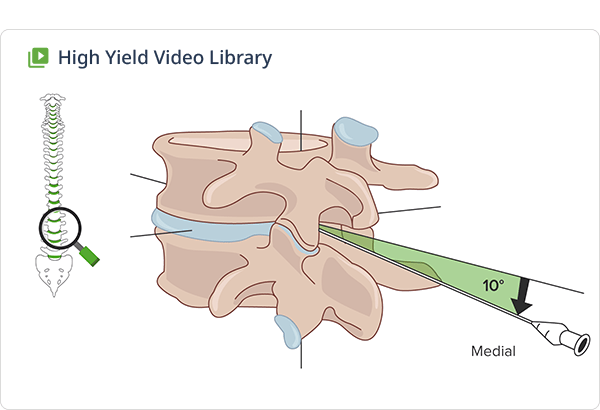
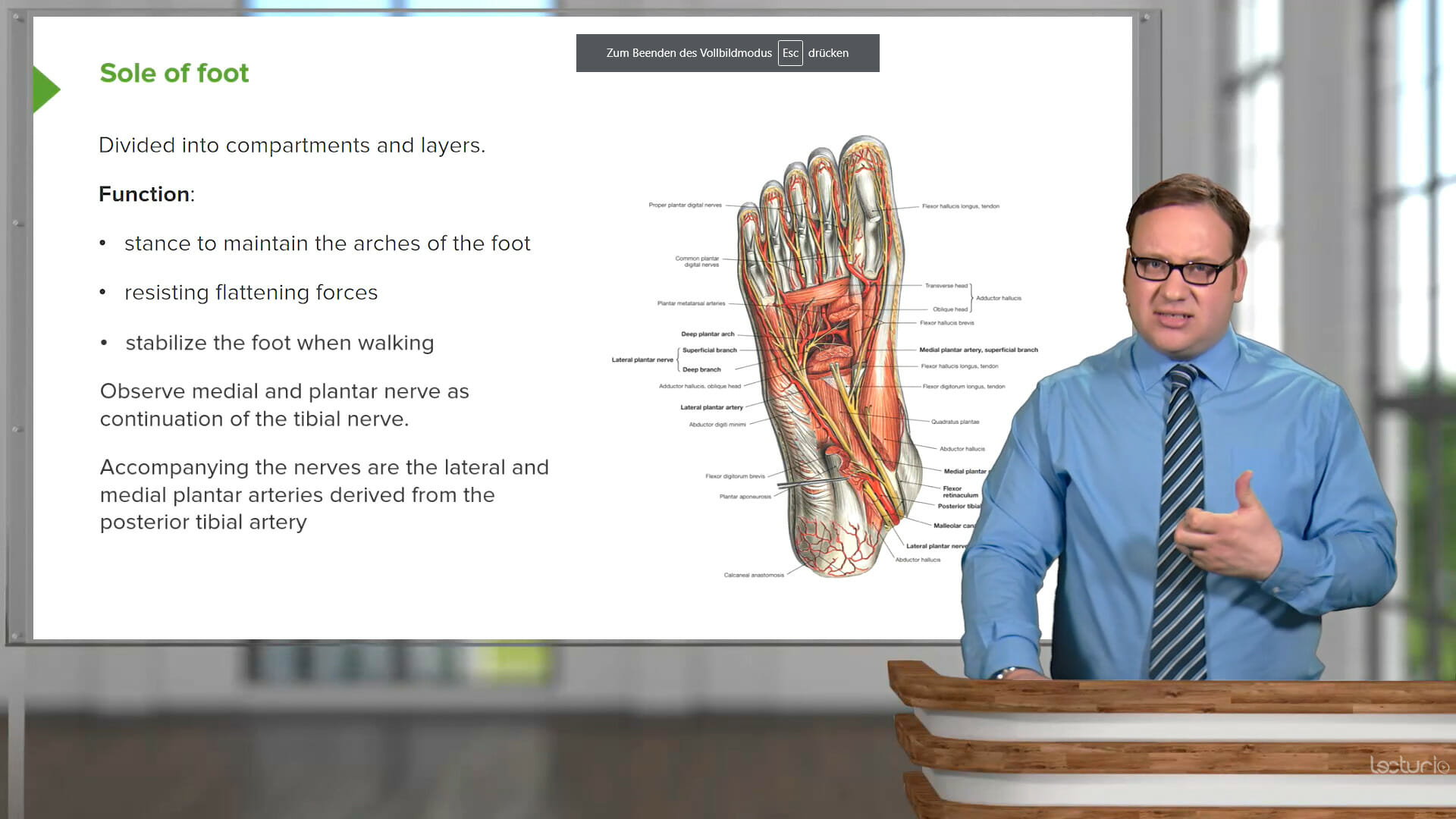
90 Anesthesiology Video Lessons
High-yield lectures with downloadable materials and multilingual subtitles
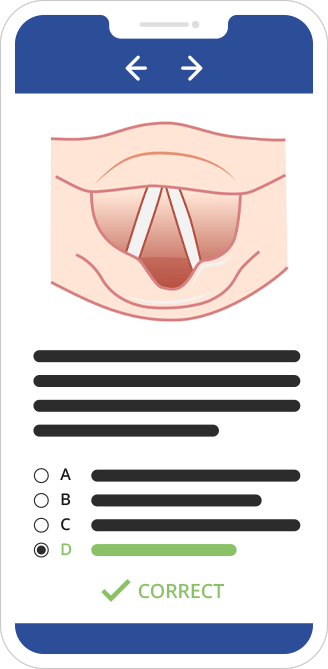
Anesthesiology Exam Practice Questions
Exam-simulating interface designed to help you become familiar with actual anesthesiology test situations
Anesthesiology Concept Pages
A comprehensive medical library to reinforce knowledge on challenging anesthesiology concepts
230 Questions for Better Recall
Adaptive learning algorithm using Spaced-Repetition quizzes for optimized long-term retention

Lecturio’s Anesthesiology Course covers all relevant topics
This top educator teaches you everything
you need to know about anesthesiology

Lecturio Medical Premium – All-in-one from day one
Let's Celebrate You Becoming a Doctor!
Save 50% on all plans now
First 7 Days Free
Save 50% on all plans now - First 7 days free
First 7 Days Free
Save 50% on all plans now - First 7 days free
Choose the plan that works for you
3 Months
/month
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Most Popular
12 Months
/month
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
24 Months
/month
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
3 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 134.97,134.97,104.97,104.97,104.97,5997,1497,74.97 charged every 3 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
Most Popular
12 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 359.88,359.88,299.88,299.88,299.88,15588,4188,215.88 charged every 12 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
24 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 599.76,599.76,479.76,479.76,479.76,23976,6216,335.76 charged every 24 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
3 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 134.97,134.97,104.97,104.97,104.97,5997,1497,74.97 charged every 3 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
Most Popular
12 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 359.88,359.88,299.88,299.88,299.88,15588,4188,215.88 charged every 12 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
24 Months
/month
1AUD,CAD,EUR,GBP,USD,INR,MXN,LUSD 599.76,599.76,479.76,479.76,479.76,23976,6216,335.76 charged every 24 months
- Full Video Library access
- Full Qbank access
- Full Concept Page Library access
- Exam-focused Learning Paths
Get full access today. Pay after 7 days. Cancel anytime.
Continue Your Learning Journey
Explore tailor-made curricula for current and future clinicians
FAQs
Anesthesiology is the medical specialty focused on making surgical, diagnostic, or other procedures painless by providing anesthesia. It involves the monitoring of vital signs and general patient well-being during procedures, critical care medicine, and pain management. Anesthesiologists may work in a variety of settings such as hospitals, surgery centers, pain clinics, and intensive care units. They have expertise in understanding, preventing, and managing complications that can arise during and after procedures.
Anesthesiology is considered moderately competitive among the medical specialties. Competitiveness can change yearly. If anesthesiology is your passion, go for it!
Anesthesiology residency typically lasts 4 years in the United States. This includes one year of internship followed by three years specifically dedicated to anesthesiology training. After residency, some may choose to pursue additional fellowship training in a sub-specialty, which can take an additional 1–2 years.
Anesthesiology assistants work under the direction of a licensed anesthesiologist to develop and implement anesthesia care plans. They are involved in various aspects of anesthesia management, including preoperative evaluation, administration of anesthesia, monitoring patients during and after anesthesia, and post-anesthesia care. Their scope of practice varies by jurisdiction and hospital policy but always involves a close working relationship with an anesthesiologist.
The most effective way to succeed in your anesthesiology class is to combine different learning modalities: First, deep-dive into the topics with video lessons hosted by competent educators followed by Lecturio’s comprehensive Concept Pages. Next, apply what you’ve learned in practical situations by answering clinical case questions in the Qbank. Lastly, make sure you retain information long-term by regularly reviewing your knowledge with the recall quizzes that come with the videos and resurface according to our smart Spaced-Repetition algorithm.
→ Create your free account here.
With your Premium membership, you get unlimited access to all video courses plus Lecturio’s Question Bank. Additionally, you will benefit from our retention quizzes designed to help you memorize key information AND Lecturio’s Study Planner to help you to schedule your study time. You can also access the unique Lecturio Bookmatcher, a tool that allows you to scan any medical textbook page to discover video lectures that will explain the topics covered — a feature that no other learning platform offers.
We’ve got four to choose from. Our 3-month plan is the most flexible option. Our 1-year plan is very popular. And our 2-year plan gives you more bang for your buck. But for the best value, our 4-year plan is hard to beat.
Tip: Sign up for Premium through our website and you’ll avoid additional app store fees. Best of all, your Premium membership is valid on all devices for the website and app!
→ Check out our plans here.
In the words of Steve Jobs: “The people who are crazy enough to think they can change the world are the ones who do.” Guarantees can only be given based on the quality of our product. Work hard and study smart with Lecturio and you will maximize recall and conceptual clarity which will significantly increase your chances of achieving high scores.




















