Fibrocystic change of the breast is a non-specific term referring to several types of benign Benign Fibroadenoma breast conditions. These are non-proliferative lesions, which include cystic and fibrous tissue formation. Fibrocystic changes Fibrocystic changes A common and benign breast disease characterized by varying degree of fibrocystic changes in the breast tissue. There are three major patterns of morphological changes, including fibrosis, formation of cysts, and proliferation of glandular tissue (adenosis). The fibrocystic breast has a dense irregular, lumpy, bumpy consistency. Examination of the Breast are seen in up to 50–60% of women, most commonly between 30–50 years of age. Changes are stimulated by both estrogen Estrogen Compounds that interact with estrogen receptors in target tissues to bring about the effects similar to those of estradiol. Estrogens stimulate the female reproductive organs, and the development of secondary female sex characteristics. Estrogenic chemicals include natural, synthetic, steroidal, or non-steroidal compounds. Ovaries: Anatomy and progesterone Progesterone The major progestational steroid that is secreted primarily by the corpus luteum and the placenta. Progesterone acts on the uterus, the mammary glands and the brain. It is required in embryo implantation; pregnancy maintenance, and the development of mammary tissue for milk production. Progesterone, converted from pregnenolone, also serves as an intermediate in the biosynthesis of gonadal steroid hormones and adrenal corticosteroids. Gonadal Hormones, and often diminish or resolve with menopause Menopause Menopause is a physiologic process in women characterized by the permanent cessation of menstruation that occurs after the loss of ovarian activity. Menopause can only be diagnosed retrospectively, after 12 months without menstrual bleeding. Menopause. Patients Patients Individuals participating in the health care system for the purpose of receiving therapeutic, diagnostic, or preventive procedures. Clinician–Patient Relationship typically present with a breast mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, “lumpy” or firm breasts Breasts The breasts are found on the anterior thoracic wall and consist of mammary glands surrounded by connective tissue. The mammary glands are modified apocrine sweat glands that produce milk, which serves as nutrition for infants. Breasts are rudimentary and usually nonfunctioning in men. Breasts: Anatomy, and/or cyclic breast pain Pain An unpleasant sensation induced by noxious stimuli which are detected by nerve endings of nociceptive neurons. Pain: Types and Pathways. The work-up involves imaging, with mammogram or ultrasound, and biopsy Biopsy Removal and pathologic examination of specimens from the living body. Ewing Sarcoma (if needed) to exclude malignancy Malignancy Hemothorax. Management includes observation, supportive measures, and altering hormone therapy, as needed. These changes do not appear to significantly increase the risk for breast cancer Breast cancer Breast cancer is a disease characterized by malignant transformation of the epithelial cells of the breast. Breast cancer is the most common form of cancer and 2nd most common cause of cancer-related death among women. Breast Cancer.
Last updated: Sep 29, 2022
Fibrocystic changes Fibrocystic changes A common and benign breast disease characterized by varying degree of fibrocystic changes in the breast tissue. There are three major patterns of morphological changes, including fibrosis, formation of cysts, and proliferation of glandular tissue (adenosis). The fibrocystic breast has a dense irregular, lumpy, bumpy consistency. Examination of the Breast typically present in reproductive-aged women as either “lumpy breasts Breasts The breasts are found on the anterior thoracic wall and consist of mammary glands surrounded by connective tissue. The mammary glands are modified apocrine sweat glands that produce milk, which serves as nutrition for infants. Breasts are rudimentary and usually nonfunctioning in men. Breasts: Anatomy,” a discrete breast mass Mass Three-dimensional lesion that occupies a space within the breast Imaging of the Breast, or mammographic abnormalities found on routine screening Screening Preoperative Care.
The most important thing is to differentiate benign Benign Fibroadenoma fibrocystic changes Fibrocystic changes A common and benign breast disease characterized by varying degree of fibrocystic changes in the breast tissue. There are three major patterns of morphological changes, including fibrosis, formation of cysts, and proliferation of glandular tissue (adenosis). The fibrocystic breast has a dense irregular, lumpy, bumpy consistency. Examination of the Breast from malignant conditions.

Mammography showing fibrocystic changes: densities typical of fibrocystic disease
Image: “Mammogram Showing Fibrocystic Disease” by National Cancer Institute. License: Public Domain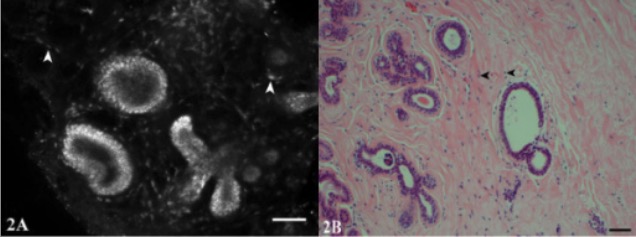
Scanning laser microscopy and hematoxylin and eosin stain (H&E) images of fibrocystic changes:
Images show the microanatomy of the branching terminal duct lobular unit and the epithelial lining of a microcyst. Fibroblasts in the surrounding stroma contain bright nuclei (arrowheads). There is dilation of ducts producing microcysts.
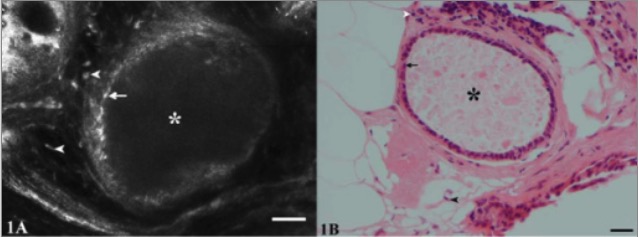
Scanning laser microscopy and hematoxylin and eosin stain (H&E) images of fibrocystic changes:
Images show the lumen of a cyst (*) lined by a layer of small, flattened epithelial cells (arrows). The nuclei of stromal cells (spindle-shaped fibroblasts and rounded lymphocytes) are evident adjacent to the cyst (arrowheads).
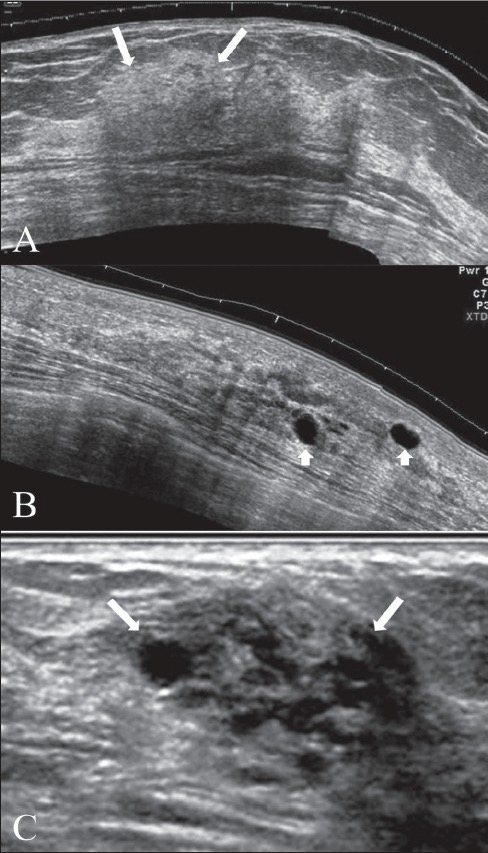
Ultrasound findings of fibrocystic change:
Extended view images (A, B) show a focal area of thickening of the breast parenchyma (A) with patchy increase in echogenicity (arrows) and scattered, discrete, thin-walled cysts (arrowheads in B). The “lump” may shows a combination of clustered tiny cysts and thickened parenchyma (arrows in C).
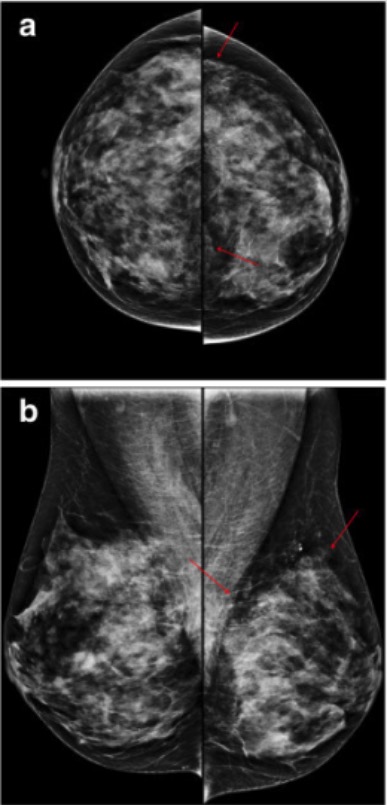
Mammography showing fibrocystic changes in the left breast of a 50-year-old woman:
Mammography craniocaudal (a) and mediolateral oblique (b) views show regional punctate or microcalcifications (arrows) in the left upper outer and inner quadrant.